
Need a chuckle or a groan? Here you go...
1. Did you hear about the guy who just found out he was color blind? It hit him right out of the purple!
2. What happened to the lab tech when he fell into the grinder? He made a spectacle of himself.
3. Why is our staff so amazing? They were all bright pupils!
4. Why did the smartphone have to wear glasses? It lost all of its contacts.
5. What did one pupil say to the other? I’m dilated to meet you.
6. What do you call a potato wearing glasses? A Spec-Tater!
7. What do you call an optician living on an Alaskan island? An optical Aleutian.
8. What was the innocent lens’s excuse to the policeman? "I’ve been framed, officer!"
9. Where is the eye located? Between the H and the J.
10. Where does bad light end up? In Prism!

Is it safe to use "Redness Relief" eye drops regularly?
The short answer is NO.
Here’s the slightly longer answer.
There are several eye “Redness Relief” products on the over-the-counter market, such as those made by Visine, Clear Eyes, and Bausch & Lomb - as well as generic versions sold by pharmacy chains.
Most commonly, the active ingredient in redness relief drops is either Tetrahydrozoline or Naphazoline. Both of these drugs are in a category called sympathomimetics.
Sympathomimetics, the active ingredient in redness relief drops, work though a process called vasoconstriction, an artificial clamping down of the superficial blood vessels on the eye surface. These blood vessels often dilate in response to an irritation. This increase in blood flow is trying to help repair whatever irritation is affecting the surface of the eye. Clamping down on those vessels by using a vasoconstrictor counteracts the body’s efforts to repair the problem.
The other downside to repetitively using redness relief drops is that after the vasoconstrictor wears off the vessels often dilate to an even larger degree than when the process started. This stimulates you to use the drops again.
All of these drops carry these same two warnings on their labels:
Do not overuse as it may produce increased redness of the eye.
Stop using and ask a doctor if you experience eye pain, changes in vision, continued redness or irritation of the eye condition worsens or persists for more than 72 hours.
Does anyone read those warnings? Almost never.
These drops are meant to be used for a VERY short duration - one or two days. That’s it!
They are not meant to be used indefinitely and they are certainly not meant to be used daily.
Take a good look at that first warning: MAY PRODUCE INCREASED REDNESS OF THE EYE.
If you are using redness relief drops repetitively you are likely making your eye redness WORSE, not better.
If you have been using redness relief drops daily you need to stop and replace them with an artificial tear or lubricating drop - something that DOES NOT say “gets the red out.”
After you make that switch your eyes are initially going to be red as your blood vessels take time to regain their normal vascular tone without the vasoconstrictor clamping down on them. The lubricating drop will actually help to repair the damage done by exposure to adverse conditions. This will decrease the inflammatory signals that make the vessels dilate. You will actually be doing something helpful to the surface of your eyes instead of just masking everything by artificially clamping down on your vessels and decreasing the flow of oxygen and nutrients to the front surface of your eye.
Using redness relief drops if you wear contacts is an even worse idea. If you put the drop in with your contact in, the contact will hold onto the drug and keep it on your eye surface longer, thus likely increasing the vasoconstriction.
Your cornea has no blood vessels in it and it depends on the blood vessels in the conjunctiva over the whites of the eye to bring in nutrients and oxygen. The other source of oxygen for the cornea is what it gets from diffusion from the atmosphere and that is also cut down by the presence of the contact lens.
The redness relief drop combined with the contact lens are now BOTH reducing the levels of oxygen getting to the cornea. Decreased oxygen to the cornea is one of the biggest risks for contact lens-related infections, including corneal ulcers.
Don’t get me wrong, I’m not condemning redness relief drops if used appropriately for a very short time to soothe the eyes if they have been temporarily exposed to elements that made them irritated. For a day or two redness relief drops are fine. But for long-term use or for use while wearing your contacts they are much more likely to cause problems than to provide any benefits.
Article contributed by Dr. Brian Wnorowski, M.D
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

We all know that during pregnancy, a woman's body goes through a great deal of change hormonally and physiologically. But did you know her eyes change as well? Below are some of the most common effects pregnancy can have on the eye.
- Corneal changes. In some cases, pregnancy can cause the cornea, the front window of the eye, to change curvature and even swell, leading to shifts in glasses and contact lens prescriptions. In addition, changes in the chemistry of the tear film can lead to dry eyes and contact lens intolerance. It is for these reasons that it is generally not recommended to have any new contact lens fitting or new glasses prescription checks until several months postpartum. We want to get the most accurate measurements possible.
- Retinal changes. Many different conditions can affect the retina during pregnancy. If the pregnant woman has diabetes, diabetic eye disease can progress by 50%. In women with preeclampsia, a condition where blood pressure rises significantly, over 40% of women can show changes in the retinal blood vessels, and 25% to 50% complain of changes to their vision.
- Eye Pressure Fluctuation. Intraocular pressure (IOP) usually decreases during pregnancy. The exact mechanism causing this is unknown, but it is usually attributed to an increase of flow of intraocular fluid out of the eye. This is good news for pregnant women with glaucoma or high IOP. In fact, the drop in IOP is larger when you start with a high IOP compared to one in the normal range.
There are many more effects that pregnancy can have on the eye, but these are the most common. One other thing to keep in mind is that though the likelihood of any adverse effect is extremely low, we try not to use any diagnostic eye drops on pregnant patients during the eye exam. Unless there is a medical necessity to dilate the pupils or check IOP, it is a good rule of thumb to put off using drops until after the patient has given birth in order to protect the developing baby.
Article contributed by Dr. Jonathan Gerard
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Alzheimer's Disease International estimates that the number of people living with dementia worldwide - nearly 44 million in 2014 - will almost double by 2030 and more than triple by 2050.
There is no single test that can show if a person has Alzheimer's, but doctors can almost always determine if a person has dementia, although it may be difficult to determine the exact cause. Diagnosing Alzheimer's requires careful medical evaluation, neurological testing, and sometimes brain imaging and blood tests to rule out other causes of dementia.
Most of the testing for early disease - MRI scans of the brain, brain PET scans looking for amyloid, and spinal taps looking for certain proteins in the spinal fluid - are not very accurate, and they are invasive and often expensive.
Researchers have now turned to findings in the eye to help with early detection and are hoping to find ways to make the diagnosis earlier when potential treatments may have a better outcome. There is also hope that these tests will be less expensive and invasive then the other options.
One of the tests that has shown promise is an OCT of the retina. Almost every eye doctor’s office already has an OCT, and so if this research proves fruitful, the test could be done relatively cheaply because there is not a need to buy more expensive equipment. The average OCT exam costs much, much less than the cost of an MRI or PET Scan.
Neuroscientists at the Gladstone Institutes in San Francisco showed a proof of concept in frontotemporal dementia, which is like Alzheimer’s but attacks much earlier and accounts for just 10% to 15% of dementia cases. They found that patients with frontotemporal dementia had thinning of the neuron layer of the retina on OCT.
In a study at Moorfields Eye Hospital they also found that people who had a thinner layer of neurons in the macula on an OCT exam were more likely to perform poorly on the cognitive tests - a clear warning sign they may be undergoing the early stages of dementia.
Study leader Dr. Fang Ko, said: “Our findings show a clear association between thinner macular retinal nerve fiber layer and poor cognition in the study population. This provides a possible new biomarker for studies of neurodegeneration.”
A second marker that is getting a careful look is identifying the presence of amyloid in the eye. Amyloid, thought to be one of the key causes of Alzheimer’s, which makes up most dementia cases, is often found to have formed into clumps and plaques in the brain. Scientists at Waterloo University in Canada found people with severe Alzheimer’s disease had deposits of a protein amyloid on their retinas.
Research conducted at Lifespan-Rhode Island Hospital in Providence co-led by Peter Snyder, a professor of neurology at Brown University, and Cláudia Santos, a graduate student at the University of Rhode Island, is attempting to detect amyloid in the retina by OCT and follows people over time to see if the amyloid increases and if it correlates with cognitive impairment.
Another angle being pursued by a company called Cognoptix is looking for amyloid in the lens of the eye. Using Cognoptix's SAPPHIRE II system, which detects amyloid in the lens, a 40-person Phase 2 clinical trial was conducted at four sites. The study recruited patients who were clinically diagnosed with probable Alzheimer’s disease (AD) via a rigorous neuropsychological and imaging workup. The study, using age-matched healthy controls, showed outstanding results of 85% sensitivity, and 95% specificity in predicting which people had probable AD.
The company planned a Phase 3 study that must show a strong correlation in a bigger study group to obtain ultimate FDA approval.
One of the other items I was going to include in this post was information on what visual symptoms occur in dementia patients and how family and friends can support them but I found an outstanding review already available online by the Alzheimer’s society that covers all those points. If you have a loved one with dementia this is an excellent read and I highly recommend you take the time to review it.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

When soft contact lenses first came on the scene, the ocular community went wild.
People no longer had to put up with the initial discomfort of hard lenses, and a more frequent replacement schedule surely meant better overall health for the eye, right?
In many cases this was so. The first soft lenses were made of a material called HEMA, a plastic-like polymer that made the lenses very soft and comfortable. The downside to this material was that it didn’t allow very much oxygen to the cornea (significantly less than the hard lenses), which bred a different line of health risks to the eye.
As contact lens companies tried to deal with these new issues, they started to create frequent-replacement lenses made from SiHy, or silicone hydrogel. The oxygen transmission problem was solved, but an interesting new phenomenon occurred.
Because these were supposed to be the “healthiest” lenses ever created, many people started to overwear their lenses, which led to inflamed, red, itchy eyes; corneal ulcers; and hypoxia (lack of oxygen) from sleeping in lenses at night. A new solution was needed.
Thus was born the daily disposable contact lens, which is now the go-to lens recommendation of most eye care practitioners.
Daily disposables (dailies) are for one-time use, and therefore there is negligible risk of overwearing, lack of oxygen, or any other negative effect that extended wear (2-week or monthly) contacts can potentially have. While up-front costs of dailies are higher than their counterparts, there are significant savings in terms of manufacturer rebates. In addition, buying contact lens solution is no longer necessary!
While a small minority of patient prescriptions are not yet available in dailies, the majority are--and these contacts have worked wonders for patients who have failed in other contacts, especially those who have dry eyes.
Ask your eye care professional if dailies might be the right fit for you.
Article contributed by Dr. Jonathan Gerard
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
What’s up with people wearing those big sunglasses after cataract surgery?
The main reason is for protection - physical protection to assure nothing hits the eye immediately after surgery, and protection from sunlight and other bright lights.
We want to protect the eye from getting hit physically because there is a small incision in the eyeball through which the surgeon has removed the cataract and inserted a new clear lens. In most modern cataract surgeries that incision is very small - about one-tenth of an inch in most cases. The vast majority of surgeons do not stitch the incision closed at the end of surgery. The incision is made with a bevel or flap so that the internal eye pressure pushes the incision closed.
The incision does have some risk of opening, especially if you were to provide direct pressure on the eyeball. Therefore, immediately after surgery we want you to be careful and make sure that you or any outside force doesn’t put direct pressure on the eye. The sunglasses help make sure that doesn’t happen while you are outside immediately after surgery. It’s the same reason that most surgeons ask you to wear a protective plastic shield over the eye at night while you are sleeping for the first week so that you don’t inadvertently rub the eye or smash it into your pillow.
The other advantage of wearing the sunglasses is to protect your eye from bright light, especially in the first day or two when your pupil may still be fairly dilated from all the dilating drops we used prior to surgery. Even after the dilation wears off, the light still seems much brighter than before your surgery. The cataracts act like internal sunglasses. The lens gets more and more opaque as the cataract worsens and so it lets less and less light into the eye. Your eye gets used to those decreased light levels and when you have cataract surgery the eye instantly goes from having all the lights dimmed by the cataract to 100% of the light getting through the new clear lens implant. That takes some getting used to and the sunglasses help you adapt early on. Think of this as if you were in a dark cave for a long period of time and then were thrust out into the bright sunlight. It would be pretty uncomfortable. The sunglasses help with that adjustment.
So why do people keep wearing those sunglasses long after their surgery? Mostly because some people really like them. They not only provide sun protection straight on, they also give you protection along the top and sides of the frame, reducing the light that can enter around the frame
If you have a spouse who wants to keep wearing those...let’s call them “inexpensive” and “less than fashionable”...sunglasses, but you’d like them to look better, there is a solution. There are sunglasses called Fitovers that go over top of your regular glasses and still provide top and side protection from the sun but look much better than the “free” ones you got for cataract surgery.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Read more: What Is the Deal with Those Weird Cataract Glasses?

Is bilberry a wonder supplement for your macular degeneration?
The jury is still out on that question. There is some supportive experimental data in animal models but no well-done human studies that show significant benefit.
What you shouldn’t do is pass up taking the AREDS 2 nutritional supplement formula, which is clinically proven to reduce the risk of severe visual loss that can happen with macular degeneration. Almost all the data supporting the POSSIBLE benefits of bilberry in visual conditions is related to NON-HUMANS. Stick with the AREDS 2 formula that has excellent clinical evidence.
So, what is bilberry and why do some people use it?
Bilberry (Vaccinium myrtillus), a low-growing shrub that produces a blue-colored berry, is native to Northern Europe and grows in North America and Asia. It is naturally rich in anthocyanins, which have anti-oxidant properties.
It is said that during World War II, British pilots in the Royal Air Force ate bilberry jam, hoping to improve their night vision. No one is exactly sure where the impetus to do this came from, but it is believed that this story is what lead to some widespread claims that bilberry was good for your eyes.
A study by JH Kramer, Anthocyanosides of Vaccinium myrtillus (Bilberry) for Night Vision - A Systematic Review of Placebo-Controlled Trials, reviewed most of the literature pertaining to the claim that bilberry improves night vision. He found that the four trials, which were all rigorous randomized controlled trials (RCTs), showed no correlation with bilberry extract and improved night vision. A fifth RCT and seven non-randomized controlled trials reported positive effects on outcome measures relevant to night vision, but these studies had less-rigorous methodology.
Healthy subjects with normal or above-average eyesight were tested in 11 of the 12 trials. The hypothesis that V. myrtillus improves normal night vision is not supported by evidence from rigorous clinical studies. There is a complete absence of rigorous research into the effects of the extract on subjects suffering impaired night vision due to pathological eye conditions.
Even though there is no solid evidence in human studies that bilberry produces any positive visual effects on night vision there is some experimental evidence that implies it might be useful in some ocular conditions whose mode of action is oxidative stress. There are recent epidemiologic, molecular and genetic studies that show a major role of oxidative stress in age-related macular degeneration.
There have been some studies showing oxidative protective effects of bilberry in non-human models.
In Protective Effects of Bilberry and Lingonberry Extracts Against Blue-light Emitting Diode Light-induced Retinal Photoreceptor Cell Damage in Vitro, Ogawa et al showed that cultured mouse cells that had bilberry extract added before subjection to high-energy short-wavelength light survived better than those that hadn't received the extract.
In Retinoprotective Effects of Bilberry Anthocyanins via Antioxidant, Anti-Inflammatory, and Anti-Apoptotic Mechanisms in a Visible Light-Induced Retinal Degeneration Model in Pigmented Rabbits, Wang et al found similarly improved survival of pigmented rabbit retinal cells when exposed to bilberry abstract prior to high-intensity light.
But bilberry is not without potential side effects.
Bilberry possesses anti-platelet activity and it might interact with NSAIDs, particularly aspirin. Excessive drinking of bilberry juice might cause diarrhea. One study of 2,295 people given bilberry extract found a 4% incidence of side effects or adverse events. Further, bilberry side effects may include mild digestive distress, skin rashes and drowsiness. Chronic uses of the bilberry leaf may lead to serious side effects. High doses of bilberry leaf can be poisonous.
Bilberry has not been evaluated by the Food and Drug Administration for safety, effectiveness, or purity.
Article contributed by Dr. Brian Wnorowski, M.D.
One of the hardest questions eye care professionals routinely have to deal with is when to tell people with visual difficulaties that they need to stop driving.
Giving up your driving privilege is difficult to come to terms with if you have a problem that leads to permanent visual decline.
The legal requirements for visual acuity vary from state to state. For example, in New Jersey the legal requirement to drive, based on vision, has been 20/50 vision or better with best correction in one eye for a “pleasure” driving license. For a commercial driving license, the requirement is 20/40 vision or better in both eyes.
In some states there is also a requirement for a certain degree of visual field (the ability to see off to the sides).
According to the Insurance Institute for Highway Safety, the highest rate of motor vehicle deaths per mile driven is in the age group of 75 and older (yes, even higher than teenagers). Much of this increased rate could be attributable to declining vision. There are also other contributing factors, such as slower reaction times and increased fragility, but the fact remains that the fatality rate is higher. , And so, when vision problems begin to occur with aging it is extremely important to do what is necessary to try to keep your vision as good as possible.
That means getting regular eye exams, keeping your glasses up-to-date, dealing with cataracts when appropriate, and staying on top of other vision-threatening conditions such as macular degeneration, glaucoma, and diabetes.
It is our responsibility to inform you when you are no longer passing the legal requirement to drive. Although not all states have mandatory reporting laws, your eye doctor will record in your medical record that you were informed that your vision did not pass the state requirements to maintain your privilege. And, yes, it is a privilege -- not a right -- to drive.
If you have a significant visual problem and your vision is beginning to decline, you need to have a frank discussion with your eye doctor about your driving capability. If you are getting close to failing the requirement, you need to start preparing with family and loved ones about how you are going to deal with not being able to drive.
Many of us eye doctors have had the unfortunate occurrence of having instructed a patient to stop driving because of failing vision, only to have him ignore that advice and get in an accident. Don’t be that person. Be prepared, have a plan.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

We have all heard the term ”Love is in the Air,” but can love really be in the eyes? Actually, Science has proven it so. Certain chemicals (or endorphins) that produce the emotion of love can be emitted through emotions expressed in the eyes. There are physiological changes in the eyes that occur when love is expressed between two individuals. Love for a romantic partner, a family member, or a favorite pet can all cause the same physical response: the pupil (black part in the center of the eye) dilates.
The size of the pupil can be an indication of emotional responses and messages. According to Scientific American, the autonomic nervous system (ANS), which directs our fight or flight response, causes the pupil to have a quick dilating response. The ANS is also in charge of heart rate and perspiration, and when a person is extremely interested in another person, the pupil has a dilating effect that is slightly less than the pupillary light reflex. This bounce in size is an automated response that gives scientists indication of mood or interest (or love) shown to a person or pet.
Mounting scientific evidence also shows the benefit of looking into the eyes of your pet, especially dogs. Stroking them causes you to become more healthy on all fronts, and a few minutes a day of lovingly looking at the dog and stroking the pet releases serotonin, prolactin, and oxytocin, which are "feel good" hormones.
There are also studies inspired by psychologist Arthur Aron, from over 20 years ago, that show if you stare into someone's eyes for 4 minutes you can fall in love... looking eye to eye allows you to connect with someone new or reminds you why you fell in love with this person in the first place.
Overall health is improved and years can be added to your life when looking at something or someone with love. Your eyes and autonomic nervous system play an intricate role in the expression of love.
Source:
12/07/2012 article of Scientific American entitled:
Why Do Pupils Dilate in Response to Emotional States?
By Joss Fong
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
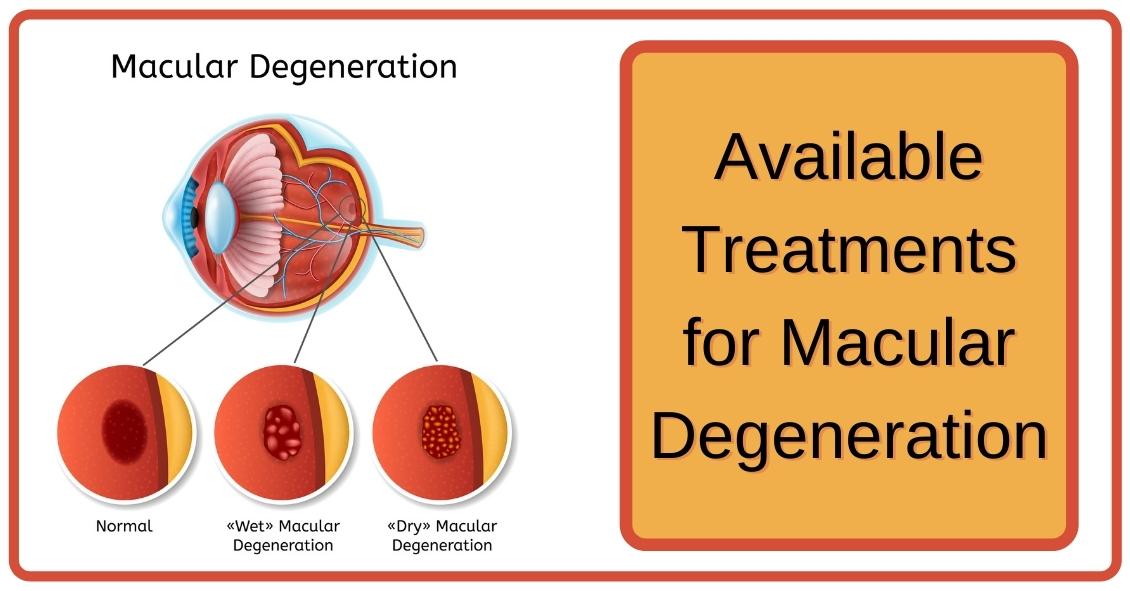
When confronted with a diagnosis of Age Related Macular Degeneration (AMD), it's natural to wonder what you should do. Here are some treatment options for both Dry and Wet Age Related Macular Degeneration.
Dry AMD Treatments
Nutrition Supplements
The Age-Related Eye Disease Study 2 (AREDS2) showed that people at high risk of developing advanced stages of AMD benefited from taking dietary supplements. Supplements lowered the risk of macular degeneration progression by 25 percent. These supplements did not benefit people with early AMD or people without AMD.
Following is the supplementation:
- Vitamin C - 500 mg
- Vitamin E - 400 IU
- Lutein – 10 mg
- Zeaxanthin – 2 mg
- Zinc Oxide – 80 mg
- Copper – 2 mg (to prevent copper deficiency that may be associated with taking high amount of zinc)
Another study showed a benefit in eating dark leafy greens and yellow, orange and other fruits and vegetables. These vitamins and minerals listed above are recommended in addition to a healthy, balanced diet.
It is important to remember that vitamin supplements are not a cure for AMD, nor will they restore vision. However, these supplements may help some people maintain their vision or slow the progression of the disease.
Wet AMD Treatments
Injection of Anti-VEGF
The most common treatment for wet AMD is an eye injection of anti-vascular endothelial growth factor (anti-VEGF). This treatment blocks the growth of abnormal blood vessels, slows their leakage of fluid, potentially helps slow vision loss, and in some cases, improves vision. There are multiple anti-VEGF drugs available: Avastin, Lucentis, and Eylea.
You may need monthly injections for a prolonged period of time for treatment of wet AMD.
Laser Treatment for Wet AMD
Some cases of wet AMD may benefit from thermal laser. This laser destroys the abnormal blood vessels in the eye to prevent leakage and bleeding in the retina. A scar forms where the laser is applied and may cause a blind spot that might be noticeable in your field of vision.
Photodynamic Therapy or PDT
Some patients with wet AMD might benefit from photodynamic therapy (PDT). A medication called Visudyne is injected into your arm and the drug is activated as it passes through the retina by shining a low-energy laser beam into your eye. Once the drug is activated by the light it produces a chemical reaction that destroys abnormal blood vessels in the retina. Sometimes a combination of laser treatments and injections of anti-VEGF mediations are employed to treat wet AMD.
Article contributed by Jane Pan M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
There have been studies undertaken over the past several years to try and understand if there are any of our day-to-day activities that either help or hurt the management of glaucoma.
Most of the studies demonstrated very little impact on the course of glaucoma. Here are some of the things researches have looked at.
Aerobic exercise: This means doing something at least four times per week for more than 20 minutes at a time that raises your pulse rate to a level that makes your heart work harder. Going from a sedentary lifestyle to active one with aerobic exercise resulted in a very slight decrease in baseline eye pressure.
Yoga: A study conducted at the Mount Sinai Health System (https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0144505) showed a significant increase in eye pressure with any head-down positioning. People with glaucoma would be wise to avoid any exercise that involves a position where your head is lower than your heart.
Weight lifting: Holding your breath while exerting yourself (called the Valsalva maneuver), is also a time when your eye pressure can go sky high. So if you lift weights for exercise, which is generally a good idea to maintain bone density, make it low weights with more repetitions of lifting, rather than heavy weights that make you grunt.
Wind instruments: A similar breath-holding problem applies to those playing the larger wind musical instruments like the French horn. One study suggested that there was a greater chance of glaucoma in symphonic wind players. If you play a brass instrument, it makes sense to have frequent checks of pressure, optic nerve head, and visual field.
Marijuana: Smoking marijuana can lower eye pressure. However, due to its short duration of action (3-4 hours), side effects, and lack of evidence that it alters the course of glaucoma, it is not recommended for glaucoma treatment.
Wearing tight neckties: This creates a very short-duration increase in eye pressure but doesn’t seem to have any long-term effects.

Ocular allergies are among the most common eye conditions to hit people of all ages.
Though typically worse in the seasons of Spring and Summer, some people suffer with allergies all year. This is especially true for people who have allergies to pet dander, mold, dust mites, and other common allergens that tend to linger throughout the year.
The hallmark sign of ocular allergies is itching.
While itching can be a symptom of other eye conditions, the likelihood that there is at least some allergy component to the condition is quite high. This seems to be particularly true when the itching occurs mainly in the inner corner of the eyes. This signals that the condition is allergy-related, whereas itching along the eyelid margin suggests other conditions.
Allergy itching is usually accompanied by redness, tearing, and string-like mucus discharge from the eye. When accompanied by rhinitis, sinusitis, and sneezing, people can truly suffer from their allergies - especially as it relates to the eye.
The good news is there are numerous avenues for relief from this annoying condition.
There are many over-the-counter antihistamine drops. Talk to your eye doctor about which ones are recommended.
In particularly severe cases, prescription antihistamine/mast cell stabilizer combination drops, or even topical steroids, can be used. In addition, cold compresses can be a great therapy in combination with the drops.
Article contributed by Dr. Jonathan Gerard
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Living an overall healthy life is good for your eyes. Healthy vision starts with healthy eating and exercise habits.
There's more to complete eye health than just carrots. Are you eating food that promotes the best vision possible? Learn what foods boost your eye well-being and help protect against diseases. Here are important nutrients to look for when selecting your foods.
- Beta carotene or Vitamin A (helps the retina function smoothly): carrots and apricots
- Vitamin C (reduce risk of macular degeneration and cataracts): citrus and blueberries
- Vitamin E (hinders progression of cataracts and AMD): almonds and sunflower seeds
- Riboflavin (helps your eyes adapt in changes in light): broccoli and bell peppers
- Lutein (antioxidant to maintain health while aging): spinach and avacado
- Zinc (transfers vitamin A to the retina for eye-protective melanin productions and helps with night vision): beans and soy beans
- DHA (helps prevent Dry Eye): Fatty fish like salmon and tuna
Keep in mind, cooked food devalues the precious live enzymes, so some of these foods are best eaten raw.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Dry eye is a very common problem that affects women more than men and becomes more prevalent as people get older.
It can present in many ways, with symptoms that can include a foreign body sensation, burning, stinging, redness, blurred vision, and dryness. Tearing is another symptom and occurs because the eye initially becomes irritated from the lack of moisture and then there is a sudden flood of tears in response to the irritation.
Unfortunately, this flood of tears can wash out other important components of the tear film that are necessary for proper eye lubrication. Signs and symptoms can range from mild to severe.
There are medications that have the potential to worsen the symptoms of dry eye. Here are some of the broad categories and specific medications that have been known to potentially worsen the symptoms:
- Blood Pressure Medications - Beta blockers such as Atenolol (Tenormin), and diuretics such as Hydrochlorothiazide.
- GERD (gastro-esophageal reflux disorder) Medications - There have been reports of an increase in dry eye symptoms by patients on these medications, which include Cimetidine (Tagamet), Rantidine (Zantac), Omerprazole (Prilosec), Lansoprazole (Prevacid), and Esomeprazole (Nexium).
- Antihistamines - More likely to cause dry eye: Diphenhydramine (Benadryl), loratadine (Claritin). Less likely to cause dry eye: Cetirizine (Zyrtec), Desloratadine (Clarinex) and Fexofenadine (Allegra). Many over-the-counter decongestants and cold remedies also contain antihistamines and can cause dry eye.
- Antidepressants - Almost all of the antidepressants, antipsychotic, and anti-anxiety drugs have the propensity to worsen dry eye symptoms.
- Acne medication - Oral Isotretinoin.
- Hormone Replacement Therapy - The estrogen in HRT has been implicated in dry eye.
- Parkinson's Medication - Levodopa/Carbidopa (Synamet), Benztropine (Cogentin), Procyclidine (Kemadrin).
- Eye Drops - In addition to oral medications many eye drops can actually increase the symptoms of dry eye, especially drops with the preservative BAK.
If you are suffering from dry eye and are using any of the medications above you should discuss this with your eye doctor and medical doctor. Don't stop these medications on your own without consulting your doctors.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

We are frequently asked if it’s wise to have cataract surgery if you have Macular Degeneration.
Let’s start with some background.
- Cataracts and Age-related Macular Degeneration (AMD) are both leading causes of visual impairment in the elderly population.
- Cataracts develop when the normal clear lens gets cloudy with age. This is correctable with cataract surgery, which involves replacing the cloudy lens with a clear, artificial lens.
- While cataracts affect the front part of the eye, AMD causes damage to the retina, which is the inner back lining of the eye.
In the past, there was a concern about cataract surgery causing progression of AMD. It was thought that there was an inflammatory component to AMD and the normal inflammatory response after cataract surgery may lead to AMD progression.
But studies have looked at patients who underwent cataract surgery compared to patients who didn't have cataract surgery and the progression of AMD was not significantly different between the two groups. However, those patients with AMD who underwent cataract surgery had a significant improvement in vision.
AMD patients can further be characterized as having wet or dry AMD, and only those with wet AMD require treatment. Patients with wet AMD need injections to decrease the growth of new blood vessels and reduce fluid in the retina.
A 2015 study showed that after cataract surgery, there was an increase in fluid in the retina of patients with wet AMD. Therefore, in patients with wet AMD, we usually want the wet AMD to be stabilized before the patient has cataract surgery. Sometimes an injection may be given prior to cataract surgery to prevent any inflammatory changes that may be associated with cataract surgery.
The majority of the studies on the subject conclude that it is safe to have cataract surgery even if you have AMD and in most cases there is a significant improvement in vision. Removing the cloudy lens also helps the ophthalmologist to better monitor the status of the AMD.
Article contributed by Dr. Jan Pan.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Read more: What About Cataract Surgery with My Macular Degeneration?
It's pretty common for eye doctors to have older patients come in asking if the white part of their eye, the sclera, has a growth or is turning a gray color.
Usually, the culprit is senile scleral plaque, which is commonly seen in people over the age of 70. It is a benign condition and more commonly seen in women. This condition is symmetrically found on both sides of the eye and is due to age-related degeneration and calcification of the eye muscle insertion into the eye. In one study, the size of the senile scleral plaque increased as the person aged and was not associated with any medical conditions. People are asymptomatic, as the plaques do not affect vision and no treatment is needed.
Another commonly asked question is: Why is the colored part of my eye turning white?
The colored part of the eye is the iris, which is covered by a clear layer called the cornea. It is actually the edge of the cornea that attaches to the white part of the eye that becomes grey or whitish colored.
This condition is called arcus senilis, which is seen in over 60% of people over the age of 60 and approximately 100% over the age of 80. There is no visual impairment and no treatment is needed. Sometimes when this condition is seen in younger patients, it may be related to high cholesterol, so a visit to the primary care doctor may be needed.
These are two very commonly encountered conditions that may cause distress for patients because it seems like their eyes are changing colors.
Thankfully, no treatment is needed for these two conditions, as they do not affect vision.
Article contributed by Dr. Jane Pan
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Recent Census Bureau data shows a population of approximately 71 million baby boomers (the generation born from 1946-1964). What does that have to do with low vision you may ask? Approximately 40 million people worldwide have some sort of blindness, and aging increases the incidence of macular degeneration and other vision impairment that qualifies them as “low vision” persons.
Low vision is a condition of the eye in which the vision falls below 20/70 in the better seeing eye. It impairs the recipients, rendering them unable to perform daily tasks that others take for granted. With this rising aging population, the awareness of low vision therapy, diagnosis, and treatments are more widely available.
Low vision treatment can help people recover from decreased visual function due to retinal disease, brain injury, neurological damage, and other causes.
It is not only the elderly population that is affected--approximately 20% of low vision patients are children under the age of 18. Childhood genetic disorders of the eye such as retinitis pigmentosa, albinism, Bests disease, ROP, rod/cone disorders, and glaucoma are among the causes of low vision in the pediatric population.
What can be done to help these millions?
There are eye care practitioners that specialize in low vision, as well as therapists. They train the patient to adjust their current lifestyles to make them more independent and utilize the current salvageable vision they do have. For example, if a person has lost their central vision due to macular degeneration, they can be trained to use their peripheral vision to accommodate for many tasks.
Because patients with low vision cannot be corrected with regular eye glasses, the use of telescopes, magnifiers, computer generated aids, training, biofeedback, and optical magnification devices are among some of the resources available to help. Occupational therapists also employ orientation and mobility assistance to help patients in their daily living skills.
There are many technologies that help to improve vision. One such technology is a bionic eye device that uses a pair of glasses with a camera that transmits video data to an implant in the back of that patients eye (the retina). This device uses technology similar to cochlear implants that stimulate auditory nerve signals to restore hearing. In the same way, visual impulses can be restored by stimulating neurons in the retina, brain, or optic nerve.
Maybe the Bionic Man TV series wasn’t too far out there and can someday be a reality............restoring vision to millions.
For more valuable information on low vision visit:
American Optometric Association AOA
American Occupational Therapy Association AOTA
American Academy of Ophthalmology AAO
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Age-related macular degeneration, often called ARMD or AMD, is the leading cause of vision loss among Americans 65 and older.
AMD causes damage to the macula, which is the central portion of the retina responsible for sharp central vision. AMD doesn't lead to complete blindness because peripheral vision is still intact, but the loss of central vision can interfere with simple everyday activities such as reading and driving, and it can be very debilitating.
Types of Macular Degeneration
There are two types of macular degeneration: Dry AMD and Wet AMD.
Dry (non-exudative) macular degeneration constitutes approximately 85-90% of all cases of AMD. Dry AMD results from thinning of the macula or the deposition of yellow pigment known as drusen in the macula. There may be gradual loss of central vision with dry AMD, but it is usually not as severe as wet AMD vision loss. However, dry AMD can slowly progress to late-stage geographic atrophy, which can cause severe vision loss.
Wet (exudative) macular degeneration makes up the remaining 10-15% of cases. Exudative or neovascular refers to the growth of new blood vessels in the macula, where they are not normally present. The wet form usually leads to more serious vision loss than the dry form.
AMD Risk factors
- Age is the biggest risk factor. Risk increases with age.
- Smoking. Research shows that smoking increases your risk.
- Family history. People with a family history of AMD are at higher risk.
- Race. AMD is more common in Caucasians than other races, but it exists in every ethnicity.
- Gender. AMD is more common in women than men.
Detection of AMD
There are several tests that are used to detect AMD.
A dilated eye exam can detect AMD. Once the eyes are dilated, the macula can be viewed by the ophthalmologist or optometrist. The presence of drusen and pigmentary changes can then be detected.
An Amsler Grid test uses pattern of straight lines that resemble a checkerboard. It can be used to monitor changes in vision. The onset of AMD can cause the lines on the grid to disappear or appear wavy and distorted.
Fluorescein Angiogram is a test performed in the office. A fluorescent dye is injected into the arm and then a series of pictures are taken as the dye passes through the circulatory system in the back of the eye.
Optical coherence tomography (OCT) is a test based on ultrasound. It is a painless study where high-resolution pictures are taken of the retina.
Article contributed by Jane Pan M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

At some point, you might be the victim of one of these scenarios: You rub your eye really hard, you walk into something, or you just wake up with a red, painful, swollen eye. However it happened, your eye is red, you’re possibly in pain, and you’re worried.
What do you do next?
Going to the Emergency Room is probably not your best bet.
Your first reaction should be to go see the eye doctor.
There are many causes for a red eye, especially a non-painful red eye. Most are relatively benign and may resolve on their own, even without treatment.
Case in point: Everyone fears the dreaded “pink eye,” which is really just a colloquial term for conjunctivitis, an inflammation or infection of the clear translucent layer (conjunctiva) overlying the white part (sclera) of our eye. Most cases are viral, which is kind of like having a cold in your eye (and we all know there is no cure for the common cold).
Going to the ER likely means you’re going to be prescribed antibiotic drops, which DO NOT treat viral eye infections. Your eye doctor may be able to differentiate if the conjunctivitis is viral or bacterial and you can be treated accordingly.
Another problem with going to the ER for your eye problem is that some Emergency Rooms are not equipped with the same instruments that your eye doctor’s office has, or the ER docs may not be well versed in utilizing the equipment they do have.
The primary instrument that your eye doctor uses to examine your eye is called a slit lamp and the best way to diagnose your red eye is a thorough examination with a slit lamp.
Some eye conditions that cause red eyes require steroid drops for treatment. NO ONE should be prescribing steroids without looking at the eye under a slit lamp. If given a steroid for certain eye conditions that may cause a red eye (such as a Herpes infection), the problem can be made much worse.
Bottom line: If you have an eye problem, see an eye doctor.
Going to the ER with an eye problem can result in long periods of waiting time. Remember, you are there along with people having heart attacks, strokes, bad motor vehicle accidents and the like-- “my eye is red” is not likely to get high priority.
Whenever you have a sudden problem with your eye your first move should be to pick up the phone and call an eye doctor. Most eye doctor offices have an emergency phone number in case these problems arise, and again, if there is no pain or vision loss associated with the red eye, it is likely not an emergency.
Article contributed by Dr. Jonathan Gerard
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
A quick explanation and background of a progressive addition lens (or PAL) is necessary in order to understand the importance of choosing the proper lens for your needs.
A progressive lens gives people an array of prescriptions - placed in the proper positions throughout the lens - to best imitate normal vision. Imagine having the precise correction needed to see a television screen more than 15 feet from you, while reading this article on your desktop computer, and then looking down at your keyboard in order to start entering the address to your favorite website. This, in a nutshell, is exactly what the progressive lens is ideally capable of accomplishing with one pair of glasses.
Having the least amount of peripheral distortion, and one of the wider ranges in both distance power, astigmatism, prism, and add power availability, we find this lens to be very versatile. The most important thing to you is that this product feels very natural in front of your eye. For first-time progressive lens wearers, there is a stigma that it takes a bit of time to adjust to a lens that holds multiple prescriptions. This is often still an issue if places use old technology lenses or don’t take careful measurements to assure the proper placement on the lens in the frame. However, with modern technology, the use of computers to fine tune this amazing product, and careful measurements and lens positioning by your optician, this lens does the best job we have seen in mimicking perfect 20/20 vision at all focal lengths.
Along with the progressive lens itself, there are other additional treatments, or “add-ons” that can immensely improve one’s experience with their glasses. These options include photochromic lenses, anti-reflective coatings, and polycarbonate scratch-resistant lenses. Talk with your eyecare team about what options might work best for you!
Article contributed by Richard Striffolino Jr.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
The word “astigmatism” is used so much in the optometric world that most people have talked about it when discussing their eye health with their doctor.
“Astigmatism” comes from the Greek “a” - meaning “without” - and “stigma” - meaning “a point.” In technical ocular terms, astigmatism means that instead of there being one point of focus in the eye, there are two. In other words, light merges not on to a singular point, but on two different points.
This is experienced in the real world by blurred, hazy vision, and can sometimes lead to eye strain or headaches if not corrected with either glasses or contact lenses.
Astigmatism is not a disease. In fact, more than 90% of people have some degree of astigmatism.
Astigmatism occurs when the cornea, the clear front surface of the eye like a watch crystal, is not perfectly round. The real-world example we often use to explain astigmatism is the difference between a basketball and a football.
If you cut a basketball in half you get a nice round half of a sphere. That is the shape of a cornea without astigmatism.
If you cut a football in half lengthwise you are left with a curved surface that is not perfectly round. It has a steeper curvature on one side and a flatter curve on the other side. This is an exaggerated example of what a cornea with astigmatism looks like.
The degree of astigmatism and the angle at which it occurs is very different from one person to the next. Therefore, two eyeglass prescriptions are rarely the same because there are an infinite number of shapes the eye can take.
Most astigmatism is “regular astigmatism,” where the two different curvatures to the eye lie 90 degrees apart from one another. Some eye diseases or surgeries of the eye can induce “irregular astigmatism,” where the curvatures are in several different places on the eye’s surface, and often the curvatures are vastly different, leading to a high amount of astigmatism.
Regular astigmatism is treated with glasses, contact lenses, or refractive surgery (PRK or LASIK). Irregular astigmatism, such as that caused by the eye disease keratoconus, usually cannot be treated with these conventional methods. In these circumstances, special contact lenses are needed to treat the condition.
The next time you hear that either you or a loved one has astigmatism, fear not.
It is easily corrected, and although astigmatism can cause your vision to be blurry, it rarely causes any permanent damage to the health of your eyes.
If you experience blurred vision, headaches, or eye strain, having a complete eye exam may lead to a diagnosis and treatment of this easily-dealt-with condition.
Article contributed by Dr. Jonathan Gerard
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Read more: Why Having Astigmatism Isn't Usually That Big a Deal

