
Transition lenses in eyeglasses have been around for many years now. The mechanics behind transition lenses is that certain chemicals in the lens interact with UV light from the sun and turn the lenses dark when you go outside and back to clear when you go inside.
This is a great accompaniment to sunglasses, as it is not always convenient to be carrying around multiple pairs of glasses with you, especially when going from inside to outside frequently. However, there are some drawbacks to transitions, including the fact that they don’t get as dark as sunglasses, have some difficulty turning dark in the car, and have a tendency to keep a slight constant tint even in dark conditions.
Vistakon, the optical wing of Johnson & Johnson, came out with the first transition contact lens a few years ago. They work well for some people, and don't seem to do a lot for others.
Just a couple personal thoughts: It can look a little strange, depending on the person and the eye color. The material itself turns gray, and therefore the person can be walking around with eyes that look darker than normal. On the plus side, though, this would be good for people limited by high prescriptions and who have difficulty with peripheral vision and glasses, yet still want the transitioning technology. On the other hand, wearing clear contact lenses with sunglasses would provide better sun coverage with the ability to remove the sunglasses when desired.
An area where transition contacts might become very useful is in outdoor sports. For any athlete who is playing an outdoor sport where the lighting conditions may change from day to day or even within a single game or event, these contacts might significantly improve the ability to perform. This is especially true in any sport where there may be significant contact or rapid head movement that can make it difficult to compete in sunglasses.
While still in its infancy, transitioning contact lenses look to be a promising technology.
Article contributed by Dr. Jonathan Gerard

For over 40 years the standard surgical treatment for glaucoma was a procedure called a trabeculectomy.
In a trabeculectomy, the ophthalmic surgeon would make a hole in the wall of eye to allow fluid from the inside of the eye to flow out of the eye and then get resorbed by the blood vessels in the conjunctiva (the mucous membrane that covers the white part of the eye).
This surgery often resulted in a large decrease in the Intraocular Pressure (IOP). Reducing the IOP is the goal of glaucoma surgery because multiple studies show that if you can reduce the pressure the progression of glaucoma slows.
The problem with trabeculectomy is that although it frequently lowers the pressure, it also has a fairly high complication and/or failure rate. This led to some reluctance to perform the procedure unless the glaucoma was severe, or the pressure was very high. As a result of those issues there has been a search during the last 40 years for something that had a lower complication rate and could be more easily deployed earlier in the disease process.
Enter Minimally Invasive Glaucoma Surgery, or MIGS. There are now several types of surgeries that fit in the MIGS category and many of them are used in conjunction with cataract surgery. They are utilized much earlier in the disease process and when combined with cataract surgery they can be used to not only help control the pressure over the long term but can often even reduce the burden of eye drops afterward.
The biggest advantage to MIGS over the trabeculectomy is that when used in conjunction with cataract surgery, MIGS can lower the eye pressure (although not as much as the trabeculectomy) but often with no higher rate of complications as there is with cataract surgery alone.
The lower complication rate is mainly because the MIGS procedures do not create a full-thickness hole in the wall of the eye. Most of them involve putting in some form of stent inside the eye. The stent lets the intraocular fluid get out of the eye more efficiently through its normal internal drain called the trabecular meshwork, rather than having to flow to the outside of the eye as with a trabeculectomy.
A stent is not the only way to lower the pressure along with cataract surgery. There is also a laser treatment you can do from the inside of the eye that slows the amount of fluid the eye makes, which also results in a lower pressure. It is called Endocyclophotocoagulation (ECP). Think of a partially clogged drain in a sink with constantly running water. If you don’t want the sink to overflow (or the pressure in the eye to get too high) you either try to unclog the drain (stent) or you turn down the faucet (ECP).
MIGS has been a great development over the last several years, enabling the surgeon to intervene at a much earlier stage of glaucoma and with a significantly lower complication rate than the more invasive trabeculectomy.
At this point I utilize one of the MIGS procedures in almost all patients who need their cataracts removed and are on one or more glaucoma medications. Even if the glaucoma is fairly well controlled at the time, the MIGS procedure gives us the opportunity to try and get a glaucoma patient off their eye drops, which is both a decreased burden of treatment and lets us keep the eye drops in reserve should the pressure start to increase again later in life.
If you have glaucoma and a cataract you should definitely discuss this with your doctor to see if a MIGS procedure along with your cataract surgery could be the right choice for you.
Article contributed by Dr. Brian Wnorowski, M.D.
Read more: What You Should Know About MIGS (Minimally Invasive Glaucoma Surgery)
If it's been a while since your last eye exam--or if you've never had one done--it's always nice to know what testing you might have done and what issues the eye doctor looks for. Here's the scoop on some common testing...
Visual Field
The visual field test is designed to check your peripheral vision, which isyour ability to see things where you are not directly looking.
When we test your vision on the basic eye chart, we are testing how well you see right in the center and it gives us no idea if you can see out away from the center. Your peripheral vision is very important because it gives you the ability to move around your environment without running into things.
There are several diseases that can severely impact your peripheral vision while leaving central vision unaffected. Some people can have perfectly normal 20/20 central visual acuity and have almost complete loss of their peripheral vision.
The main culprits that can have a big impact on your peripheral vision are glaucoma, some retinal diseases such as retinal detachments or retinitis pigmentosa, and some neurological problems like brain tumors, strokes, pseudotumor cerebri, and multiple sclerosis.
Most visual field tests are now done on an automated machine that flashes lights in your peripheral vision while you stare straight ahead. The lights continue to get dimmer until you can no longer detect that they are there. The machine is trying to find the dimmest light you can see at each point in your peripheral vision that it is testing for.
Many patients get anxious when they take this test because everyone wants to do well on it. That sometimes results in people not staring straight ahead but trying to look around to find the lights in an effort to do better.
That just makes the test come out worse. The machine also makes some noise as it changes location of the test light. Some people start pressing the buzzer whenever they hear a noise. They think there must be a light they missed but the machine, several times during the test, makes noise and then doesn’t put a light on to specifically see if you are trying to cheat by hitting the buzzer on the noise rather that seeing the light. Please don’t do those things - you are only cheating yourself and making it more difficult to figure out your problem.
Ocular Coherence Tomography (OCT)
The OCT really took hold in eye doctors' offices at the beginning of this century. It was the first time we were able to see anatomy and pathology inside the eye on a microscopic level without the use of any radiation.
It has been a great addition to our examination techniques and allowed us to see many causes of vision loss at a level of detail we never had before.
The two biggest uses for OCT in optical health are diagnosing diseases of the retina, particularly the area of central vision called the macula, and for diseases of the optic nerve, the most common of which is glaucoma.
For retinal disease it has been extremely helpful for macular problems such as macular degeneration (the leading cause of blindness in the U.S.), diabetic retinopathy, retinal vascular occlusions, and retinal swelling from inflammation.
The OCT allows us to see the individual cellular levels of the retina and helps in diagnosing the exact level where the pathology is occurring. If you look into the eye at the retina and see some bleeding in the macula it is difficult to judge where that blood exists. Is it superficial in the retina and coming from the retinal circulation or is it deep in and coming from the choroidal circulation under the retina?
The difference between those two locations can have a significant impact on what disease is causing the problem and what the proper treatment is. The OCT is also helpful in following the effect of treatment. If you are treating a bleeding or swelling problem in the retina, the OCT can track the degree of improvement with a level of detail that could never be matched by the human eye.
For glaucoma and other problems with the optic nerve, the OCT can precisely measure the thickness of the nerve tissue as it passes through the optic nerve. The hallmark of glaucoma is progressive loss of nerve fibers in the optic nerve. Being able to measure the nerve thickness down to the micron level assists in both diagnosing and watching for progression of any optic nerve disease.
Fundus Photography
A picture is worth 1,000 words...
Fundus photography is just that, a regular picture of the inside of your eye. The pictures highlight the appearance of the macula and the optic nerve and record it for prosperity.
As eye doctors we make notes in the medical record of what we see when we look in the eye. The wording of anything that looks abnormal with the retina or optic nerve does vary somewhat from doctor to doctor. One of things we record is something called the cup to disk ratio (C:D) of the optic nerve. We express that ratio as a percentage. Normal is about 30% or .3. The range of normal is very wide and some “normal” eyes have a .1 cup and others can have a .7.
In glaucoma those percentages get larger over time as the person loses nerve tissue. So, if you were born with a .3 cup but in your 60’s you were found to have a .5 cup that would be a strong indicator that you might have glaucoma. However, if you were born with a .5 cup and at 60 you still have a .5 cup then you don’t have glaucoma. When you look at someone at 60 with a .5 cup it’s hard to be sure if this is normal for that person or did they progress from a .3 cup to a .5 cup. If only I had a picture …
Pictures of the back of the eye really do tell the story better than words. I can describe what the C:D looks like to me but a different doctor may describe it differently. Doctors are usually fairly consistent in their estimate of the C:D when it is the same doctor watching that C:D over time. When a different doctor estimates the C:D that consistency is just not there. My .4 C:D may be my partner’s .5. But you can’t argue with the picture.
The same thing occurs with retinal bleeding. Rating the amount of bleeding as mild, moderate, or severe is somewhat helpful but there is a broad range of “mild” or “moderate”. When comparing two pictures taken at two different points of time it is much easier to decide if something is really getting better or worse.
We also use fundus photography to keep an eye on small tumors, called choroidal nevi, that can develop in the eye. These are increased areas of pigmentation under the retina in an area called the choroid. Most eye doctors explain these pigmented spots as “freckles in the eye.” Most choroidal nevi are small and fairly flat. They can, however, sometimes grow larger and rarely turn into a melanoma in the eye. Serial photographs are very helpful in watching the lesions for growth.
These three tests - visual field, OCT, and fundus photography - make up the core of our testing. There are many other tests that can be performed along with your eye exam but these three we described here probably make up about 80% of the tests you may encounter, depending on your eyes.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Lyme disease is an infection that is caused by a spirochete (a type of microorganism) called Borrelia burgdorferi, and more rarely by Borrelia mayonii. It is transmitted to humans by the bite of a deer tick.
The disease has a strong geographical incidence, being highly concentrated in the Northeastern United States and also in Minnesota and Wisconsin. However, the tick's habitat has been spreading rapidly, and it is always a good idea to be cautious and consult medical help if you think you might have been bitten by a tick that could possibly be infected.
Lyme disease was first recognizedin the area of Lyme, Connecticut, in 1975. It can start with a characteristic “bull’s eye” rash, in which there is a central spot that is surrounded by clear skin that is then ringed by an expanding rash. It can also appear just as an expanding rash.
This rash usually starts within days of the tick bite. Eye problems can occur along with this rash in the first phase of the disease. This includes red eyes that can look like full-blown pink eye, along with eyelid swelling. It also can produce iritis or uveitis, which include sensitivity to light and inflammation inside the eye.
The second phase of the disease usually starts within a few weeks of the tick bite and this occurs because the spirochete gets into the blood stream. This stage often has rashes starting away from the original bite site. It can also produce joint pain, weakness, and inflammation in several organs including the heart, spleen, liver and kidneys.
There are also several ways the second phase can affect your eyes. It can cause inflammation in your cornea (keratitis), retina (retinitis), optic nerve (optic neuritis), uvea (uveitis), the jelly-like vitreous (vitritis) that fills the back of the eye, and the muscles that move your eye around (orbital myositis). It can also affect the eye if it causes problems with the nerve that controls your eyelid muscles so that your eye will not close properly (Bell’s palsy).
There is a third phase of the disease that is caused by long-term persistent infection. This phase can create multiple neurologic problems and can appear very similar to the presentation of Multiple Sclerosis (MS). The eyes can show any of the same signs as phase two, but the most common presentation is persistent keratitis. Keratitis symptoms are an inflamed cornea, often accompanied by significant pain, light sensitivity, a gritty feeling, and sight impairment.
The diagnosis is made through observation of the presenting symptoms, location in an area where there are significant numbers of the disease-carrying ticks, and a blood test that can confirm the diagnosis.
The symptoms and signs of Lyme disease can mimic many other problems, so it is important to keep Lyme disease in mind if you are having multiple problems involving different organs and you know or have any suspicion that you may have had a tick bite while you were in areas where the disease is prevalent.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

A common question asked during the eye exam is, “When is the puff coming?”
Patients are referring to air-puff or non-contact tonometry. Tonometry is the procedure used to measure eye pressure, and this is important for diagnosing and monitoring glaucoma.
In non-contact tonometry, a puff of air is used to measure the pressure inside the eye. The benefit of this test is there is no actual contact with the eye, but the air puff is sometimes very startling for patients. Some people hate that test and it isn’t the most accurate way to measure your eye pressure.
Some doctors don’t even use the air-puff test. Instead, they place a yellow drop that consists of a numbing medicine and then shine a blue light on the eye. This is done in front of the slit lamp and a small tip gently touches the eye to measure the eye pressure. This procedure is called Goldmann tonometry and is considered the gold standard for measuring eye pressure.
Another method for checking eye pressure is the Tonopen. This is a portable, hand-held instrument that is useful when patients can’t sit in front of the slit lamp to have their eye pressure checked. The Tonopen also requires a numbing drop to be placed in the eye, and the tip gently touches the eye.
A common question related to tonometry is “what normal eye pressure?”
Normal eye pressure ranges from 10-21 mm Hg. Eye pressure doesn't have any relationship to blood pressure. Many times, people are surprised that their eye pressure is high, but they have normal blood pressure. In general, there is no diet or exercise that will significantly affect eye pressure. It is therefore important to have your eye pressure checked regularly because there are usually no symptoms of high eye pressure until it has affected your vision.
Article contributed by Dr. Jane Pan
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
We sometimes get asked, "Why do I need an eye exam when I can see great?"
An eye exam doesn't just check your visual acuity--we are also looking for a number of treatable eye diseases that have few or no visual symptoms in their early stages. In fact, the three leading causes of legal blindness in the United States all start with almost no visual symptoms detectable by the person wit the disease. The three diseases are macular degeneration, glaucoma, and diabetic retinopathy. Each of these diseases gets more prevalent as people age. That is why regular eye exams are recommended to become more frequent as adults get older.
Macular Degeneration: The leading cause of legal blindness in the United States is a treatable--but not curable--disease. Early detection and treatment can significantly improve the long-term outcome. In the earliest stages, often when people are unaware that they have a problem, treating the disease with a very specific vitamin regimen called AREDS 2 can help. These vitamins have been shown to slow the progression of the disease and to improve long-term outcomes. When the disease becomes more advanced there is the possibility of bleeding in the retina. If left untreated, that almost always results in severe visual loss. There now are several medications that, when injected into the bleeding eye, can arrest the bleeding and potentially improve vision.
Glaucoma: The second leading cause of legal blindness in the United States is often called "the silent thief of sight." With glaucoma, there can be severe damage to the optic nerve before a person recognizes he is having a problem. Usually by the time a person notices symptoms, 70% of the optic nerve is destroyed. As of now, once that damage has occurred it cannot be reversed. This makes early diagnosis absolutely critical to saving your sight. In most cases (but not all) early detection and treatment can preserve functional vision throughout your lifetime.
Diabetic Retinopathy: This is another leading cause of legal blindness that has no visual symptoms until the disease is in its advanced stages. Every diabetic should have an annual eye exam to check for signs of retinal disease. If detected and treated in its early stages, the disease can usually be controlled and the vision preserved.
As you can see, there are very strong reasons to have your eyes examined regularly in order to keep good visual health and function throughout your lifetime.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

An old Creek Indian proverb states, "We warm our hands by the fires we did not build, we drink the water from the wells we did not dig, we eat the fruit of the trees we did not plant, and we stand on the shoulders of giants who have gone before us."
In 1961, the Eye Bank Association of America (EBAA) was formed. This association stewards over 80 eye banks in the US with over 60,000 recipients each year of corneal tissue that restores sight to blind people. Over one million men, women, and children have had vision restored and pain relieved from eye injury or disease. The Eye Bank Association of America is truly a giant whom shoulders that we stand upon today. Their service and foresight into helping patients with blindness is remarkable.
It is important to give back the gift of sight. You may be asking, “how does this affect me?” On the back of your drivers license form there is a box that can be checked for being an organ donor. Many people forego this option because they are not educated on the benefits of it. There are many eye diseases that rob people of sight because of an opacity, pain, or disease process of the cornea. Keratoconus, a disease that causes malformation of the curvature of the cornea, can be treated by a corneal transplant. Chemical burns that cause scarring on the cornea leave people blinded or partially blind. This is another condition that requires a corneal transplant.
When it comes to corneal tissue, virtually everyone is a universal donor, because the cornea is not dependent on blood type. Corneal transplant surgery has a 95% success rate. According to a recent study by EBAA, eye disorders are the 5th costliest to the US economy behind heart disease, cancer, emotional disorders, and pulmonary disease. The cost is incurred when the person, for example, is a working age adult and can no longer hold a job because of vision issues. The gift of a corneal transplant can be one way to restore not only their vision, but their way of life, and their contribution to society.
By becoming a donor, or educating others to consider being an organ donor, you can give the gift of sight to someone on a waiting list. When you educate others to give the precious gift of sight, you become a giant whose shoulders others can stand on. Become a donor today.
For more information go to www.restoresight.org or contact your local drivers license office.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
In light of the holiday season, here are our top 10 eye care jokes.
1) What do you call a blind deer? No Eye Deer!
2) What do you call a blind deer with no legs? Still No Eye Deer!
3) Why do eye doctors live long lives? Because they dilate!
4) Why did the blind man fall into the well? He couldn’t see that well.
5) Why shouldn’t you put avocados on your eyes? Because you might get guac-coma!
6) What did the right eye say to the left eye? "Between you and me, something smells."
7) A man goes to his eye doctor and tells the receptionist he’s seeing spots. The receptionist asks if he’s ever seen a doctor. The man replies, “No, just spots.”
8) How many eye doctors does it take to screw in a light bulb? One … or two
9) Unbeknownst to her, a woman was kicked out of peripheral vision club. She didn’t see that one coming!
10) What do you call a blind dinosaur? A do-you-think-he-saurus
Bonus: What do you call a blind dinosaur’s dog? A do-you-think-he-saurus rex!
Article contributed by Dr. Jonathan Gerard
Punctal plugs are something we use to help treat Dry Eye Syndrome.
This syndrome is a multifactorial problem that comes from a generalized decrease in the amount and quality of the tears you make. There is often both a lack of tear volume and inflammation in the tear glands, which interfere with tear production and also cause the quality of the tears to not be as good.
We make tears through two different mechanisms. One is called a basal secretion of tears, meaning a constant low flow or production of tears to keep the eye moist and comfortable. There is a second mechanism called reflexive tear production, which is a sudden flood of tears caused by the excitation of nerves on the eye surface when they detect inflammatory conditions or foreign body sensations. It is a useful reflexive nerve loop that helps wash out any foreign body or toxic substance you might get in the eye by flooding the eye with tears. Consider what happens when you get suntan lotion in your eye. The nerves detect the irritation that the lotion creates, and your eyes quickly flood with tears.
That reflex mechanism is how some people get tearing even though the underlying cause of that tearing is dry eye. They don’t produce enough of the basal tears, the eye surface gets irritated and then the reflex tearing kicks in and floods their eyes, tearing them up. Once that reflex is gone then the eye dries out again and the whole cycle starts over.
One of the treatments for dry eyes is to put a small plug into the tear drainage duct so that whatever tears you are making stay on the eye surface longer instead of draining away from the eye into to the tear drainage duct and emptying into your nose.
There are several different types of punctal plugs. Some are made of a material that is designed to dissolve over time. Some materials dissolve over two weeks, while others can last as long as 6 months. There are also plugs made out of a soft silicone material that are designed to stay in forever. They can, however, be removed fairly easily if desired or they can fall out on their own, especially if you have a habit of rubbing near the inside corner of your eye.
One of the big advantages of punctal plugs is that they can improve symptoms fairly rapidly - sometimes as quickly as a day.
The long-term medical treatment for dry eyes such as Restasis, Xiidra or the vitamin supplement HydroEye can take weeks or months to have a good effect.
On the other hand, plugs simply make you retain your tears for a longer time; they don’t help the underlying inflammation. That is where the medical treatment comes in. Sometimes it is useful to use a temporary plug for more instant relief while you are waiting for the medical treatment to work. Sometimes there is clearly just a deficiency of tears and not much inflammation and the plugs alone will improve your symptoms.
All in all, punctal plugs are a safe, effective, and relatively easily-inserted treatment for dry eyes.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Have you ever seen a temporary black spot in your vision? How about jagged white lines? Something that looks like heat waves shimmering in your peripheral vision?
If you have, you may have been experiencing what is known as an ocular migraine. Ocular migraines occur when blood vessels spasm in the visual center of the brain (the occipital lobe) or the retina.
They can take on several different symptoms but typically last from a few minutes to an hour. They can take on either positive or negative visual symptoms, meaning they can produce what looks like a black blocked-out area in your vision (negative symptom), or they can produce visual symptoms that you see but know aren’t really there, like heat waves or jagged white lines that look almost like lightning streaks (positive symptoms).
Some people do get a headache after the visual symptoms but most do not. They get the visual symptoms, which resolve on their own in under an hour, and then generally just feel slightly out of sorts after the episode but don’t get a significant headache. The majority of episodes last about 20 minutes but can go on for an hour. The hallmark of this problem is that once the visual phenomenon resolves the vision returns completely back to normal with no residual change or defect.
If you have this happen for the first time it can be scary and it is a good idea to have a thorough eye exam by your eye doctor soon after the episode to be sure there is nothing else causing the problem.
Many people who get ocular migraines tend to have them occur in clusters. They can have three or four episodes within a week and then may not have another one for several months or even years.
There are some characteristics that raise your risk for ocular migraines. The biggest one is a personal history of having migraine headaches. Having a family history of migraines also raises your risk, as does a history of motion sickness.
Although the symptoms can cause a great deal of anxiety, especially on the first occurrence, ocular migraines rarely cause any long-term problems and almost never require treatment as long as they are not accompanied by significant headaches.
So if symptoms like this suddenly occur in your vision, try to remain calm, pull over if you are driving, and wait for them to go away. If they persist for longer than an hour, you should seek immediate medical attention.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Read more: These weird spots and jagged lines are scaring me!

Not everyone understands the importance of sunglasses when the weather turns cold.
Polarized sunglasses are usually associated with Summer, but in some ways it is even more important to wear protective glasses during the Winter.
It’s getting to be that time of year when the sun sits at a much different angle, and its rays impact our eyes and skin at a lower position. This translates to an increase in the exposure of harmful UV rays, especially if we are not wearing the proper sunglasses as protection.
Polarized sunglasses, which are much different than the older dye-tinted lenses, are both anti-reflective and UV resistant. A good-quality polarized sunglass lens will protect you from the entire UV spectrum. This not only preserves your vision, but it also protects the skin around the eyes, which is thought to have a much higher rate of susceptibility to skin cancer.
Snow poses another issue that can be countered by polarized sunglasses.
Snow on the ground tends to act as a mirror because of its white reflective surface and this reflection can become a hindrance while driving. The anti-reflective surface of polarized sunglasses helps reduce the glare and gives drivers improved visibility.
Polarized sunglasses come in many different options based on a patient’s needs. Whether it’s single-vision distance lenses, bifocals, or progressive lenses, there is a polarized lens for every patient.
Winter is a great time of year to ask your optical department about purchasing polarized sunglasses.
Article contributed by Richard Striffolino Jr.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Now that you have picked up your new pair of prescription eyeglasses, your focus should become taking care of them. This is a task many disregard, but it is imperative that you make sure you are following a couple simple steps to keep the quality of your vision with your new spectacles.
We are all guilty of using a garment when in a rush to wipe away a pesky smudge on our glasses. This act is unfortunately the worst thing you can do for your lenses.
No matter how clean your clothes are, dust particles and even small bits of sand and debris cling to them. Since eyeglass lenses are not made of diamonds, these tiny little particles can do tremendous amounts of damage to your new lenses. The smallest little crumb can grind a scratch directly in your line of vision, which in turn can render your glasses almost useless.
Most of us know what it feels like trying to concentrate on the world in front of you when there is a little scratch distorting and distracting your vision. A majority of the time, these little scratches can be avoided by following a few simple steps.
You may have noticed while shopping in your favorite store that they sell a variety of eyeglass cleaners. You need to be careful because the sprays and wipes which you can purchase in retail stores are not necessarily approved for all types of eyeglass lens materials.
This factor makes them fall under that category of products that many eye care professions cannot recommend. Most of these liquids contain a form of acetone or other cleaning agent that is too harsh for plastic lenses. Many years ago, when all eyeglasses were actually made out of crown glass, these products would have worked just fine. Now, during a time where they have developed thinner, lighter materials like cr-39 plastic and polycarbonate, these products have proven to be too hard on the lenses.
Over time, the lenses will start to break down if exposed to the chemicals used in these sprays, causing a fogging effect. Once again, you are left with a pair of glasses that are now unable to be worn.
Now that we have gone over the two main culprits in the destruction of eyeglass lenses, other than accidents, let’s focus on some tips to extend the life of your glasses.
Most importantly, you should use an eyeglass case. For the large portion of patients who wear their glasses all day, it’s understandable how awkward it can be to carry a case around. But it’s nowhere near as frustrating as realizing the new pair of eyeglasses you just purchased is becoming scratched and ruined.
Also, you do not need to carry the case with you everywhere you go. Strategically leaving a case on a bedside table, in your car, or in a purse is the difference between “life or death” for your glasses.
There is also a simple way to clean your glasses that does not require you to purchase anything you probably don’t already have at home. Using lukewarm water at the sink, place a small, pea-sized dab of dish soap on your fingers. Gently rub the soap on both lenses from side to side, and then rinse with warm water. Use a clean microfiber cloth to dry your glasses.Taking care of your glasses today means you have them for clear vision tomorrow and into the future.
Article contributed by Richard Striffolino Jr.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

The American Optometric Association has recommendations for how often adults need to get their eyes examined and those recommendations vary according to the level of risk you have for eye disease.
| Patient age (years) | Asymptomatic/low risk | At-risk |
| 19 through 40 | At least every two years | At least annually, or as recommended |
| 65 and older | Annually | At least annually or as recommended |
As you can see, the guidelines recommend more frequent exams as you get older. Here are the TOP 4 REASONS why you need your eyes examined more frequently as you get older:
1. Glaucoma
Glaucoma is the second leading cause of blindness in the United States. It has no noticeable symptoms when it begins and the only way to detect glaucoma is through a thorough eye exam. Glaucoma gets more and more common as you get older. Your risk of glaucoma is less then 1% if you are under 50 and over 10% if you are 80 or over. The rates are higher for African Americans. Glaucoma can be treated but not cured. The earlier it is detected and treated, the better your chances for keeping your vision.
2. Macular Degeneration
Macular degeneration is the leading cause of blindness in the U.S. Like glaucoma, it gets more common as you age. It affects less than 2% of people under 70, rises to 10% in your 80s and can get as high as 50% in people in their 90s. The rates are highest in Caucasians. Macular degeneration can also be treated but not cured. Early intervention leads to better outcomes.
3. Cataracts
As in the cases above, cataracts get more common as you get older. If they live long enough, almost everyone will develop some degree of cataracts. In most people, cataracts develop slowly over many years and people may not recognize that their vision has changed. If your vision is slowly declining from cataracts and you are not aware of that change it can lead to you having more difficulty in performing life’s tasks. We get especially concerned about driving since statistics show that you are much more likely to get in a serious car accident if your vision is reduced. There is also evidence that people with reduced vision from cataracts have a higher rate of hip fractures from falls.
4. Dry Eyes
Dry eyes can affect anyone at any age but the incidence tends to be at its highest in post-menopausal women. Dry eyes can present with some fairly annoying symptoms (foreign body sensation in the eye, burning, intermittent blurriness). Sometimes there aren’t any symptoms but during an exam we can see the surface of the cornea drying out. Dry eye can lead to significant corneal problems and visual loss if it gets severe and is left untreated.
One of the most heart-breaking things we see in the office is the 75-year-old new patient who hasn’t had an eye exam in 10 years and he comes in because his vision “just isn’t right” and his family has noticed he sometimes bumps into things. On exam, his eye pressures are through the roof and he is nearly blind from undetected glaucoma. And at that point there is no getting back the vision he has lost. If he had only come in several years earlier and just followed the guidelines, all this could have been prevented. Now he is going to have to live out the rest of his years struggling with severe vision loss.
DON’T LET THAT BE YOU!!!!!!
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Read more: 4 Good Reasons for Older Adults to Have Regular Eye Exams
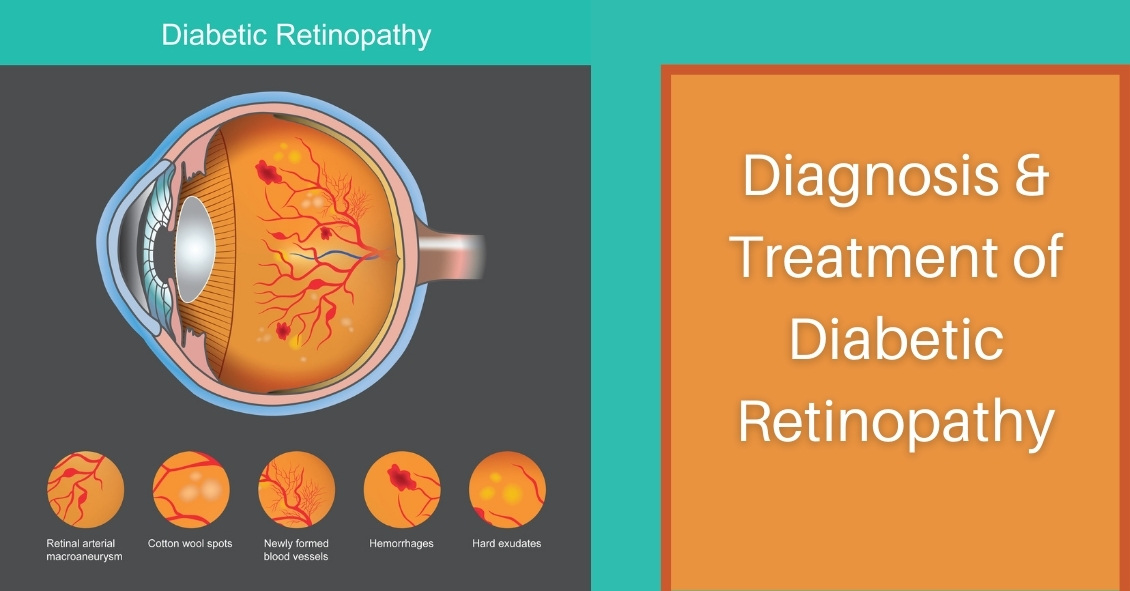
Diabetic retinopathy is an eye condition that can affect the retina of people who have diabetes.
The retina is the light-sensitive tissue that lines the back of the eye, and it detects light that is then processed as an image by the brain. Chronically high blood sugar or large fluctuations in blood sugar can damage the blood vessels in the retina. This can result in bleeding in the retina or leakage of fluid.
Diabetic retinopathy can be divided into non-proliferative or proliferative diabetic retinopathy.
Non-proliferative diabetic retinopathy: In the early stage of the disease, there is weakening of the blood vessels in the retina that causes out-pouching called microaneurysms. These microaneurysms can leak fluid into the retina. There can also be yellow deposits called hard exudates present in the retina from leaky vessels.
Diabetic macula edema is when the fluid leaks into the region of the retina called the macula. The macula is important for sharp, central vision needed for reading and driving. The accumulation of fluid in the macula causes blurry vision.
Proliferative diabetic retinopathy: As diabetic retinopathy progresses, new blood vessels grow on the surface of the retina. These blood vessels are fragile, which makes them likely to bleed into the vitreous, which is the clear gel that fills the middle of the eye. Bleeding inside the eye is seen as floaters or spots. Over time, scar tissue can then form on the surface of the retina and contract, leading to a retinal detachment. This is similar to wallpaper contracting and peeling away from the wall. If left untreated, retinal detachment can lead to loss of vision.
Symptoms of diabetic retinopathy:
- Asymptomatic: In the early stages of mild non-proliferative diabetic retinopathy, the person will usually have no visual complaints. Therefore, it is important for people with diabetes to have a comprehensive dilated exam by their eye doctor once a year.
- Floaters: This is usually from bleeding into the vitreous cavity from proliferative diabetic retinopathy.
- Blurred vision: This can be the result of fluid leaking into the retina, causing diabetic macular edema.
Risk factors for diabetic retinopathy:
- Blood sugar. Lower blood sugar will delay the onset and slow the progression of diabetic retinopathy. Chronically high blood sugar and the longer the duration of diabetes, the more likely chance of that person having diabetic retinopathy.
- Medical conditions. People with high blood pressure and high cholesterol are at greater risk for developing diabetic retinopathy.
- Ethnicity. Hispanics, African Americans, and Native Americans are at greater risk for developing diabetic retinopathy.
- Pregnancy. Women with diabetes could have an increased risk of developing diabetic retinopathy during pregnancy. If they already have diabetic retinopathy, it might worsen during pregnancy.
Article contributed by Jane Pan M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Read more: Diabetic Retinopathy Must-Knows for Everyone with Diabetes
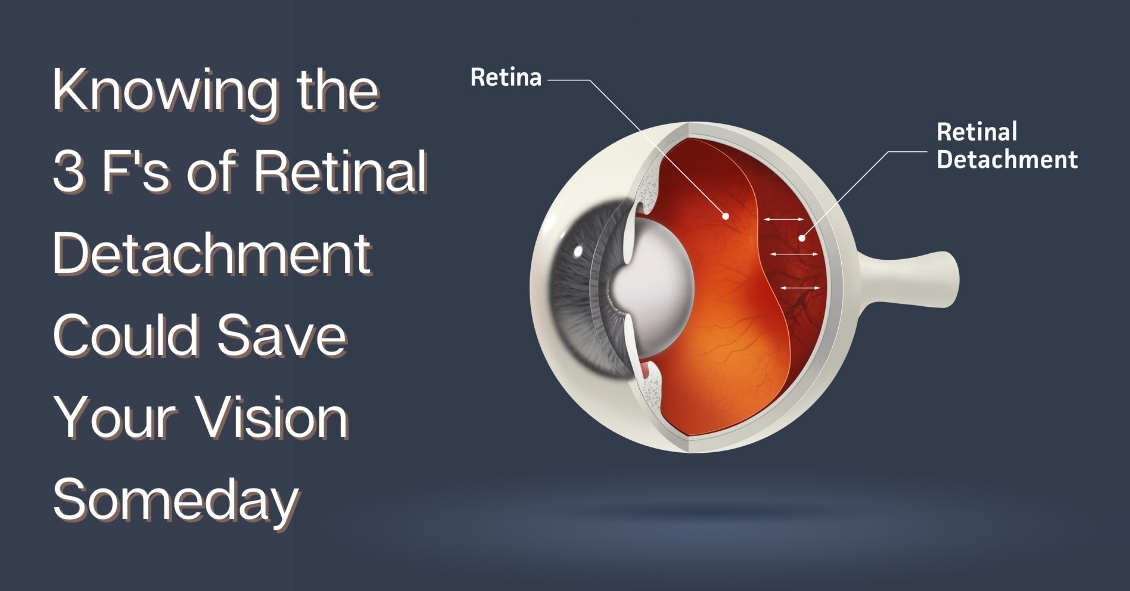
If you are seeing the 3 F's, you might have a retinal tear or detachment and you should have an eye exam quickly.
The 3 F's are:
- Flashes - flashing lights.
- Floaters - dozens of dark spots that persist in the center of your vision.
- Field cut – a curtain or shadow that usually starts in peripheral vision that may move to involve the center of vision.
The retina is the nerve tissue that lines the inside back wall of the eye and if there is a break in the retina, fluid can track underneath the retina and separate it from the eye wall. Depending on the location and degree of retinal detachment, there can be very serious vision loss.
If you have a new onset of any of the three symptoms above, you need to get in for an appointment fairly quickly (very quickly if there are two or more symptoms).
If you have just new flashes or new floaters you should be seen in the next few days. If you have both new flashes and new floaters or any field cut, you should be seen in the next 24 hours.
When you go to the office for an exam, your eyes will be dilated. A dilated eye exam is needed to examine the retina and the periphery. This may entail a scleral depression exam where gentle pressure is applied to the outside of the eye to examine the peripheral retina. Some people have a hard time driving after dilation--since the dilating drops may last up to 6 hours, you may want to have someone drive you to and from your appointment.
If the exam shows a retina tear, treatment would be a laser procedure to encircle the tear.
If a retinal tear is not treated in a timely manner, then it will progress into a retinal detachment. There are four treatment options for retinal detachment:
- Laser. A small retinal detachment can be walled off with a barrier laser to prevent further spread of the fluid and the retinal detachment.
- Pneumatic retinopexy. This is an office-based procedure that requires injecting a gas bubble inside the eye. The patient then needs to position his or her head for the gas bubble to reposition the retina back along the inside wall of the eye. A freezing or laser procedure is then performed around the retinal break. This procedure has about 70% to 80% success rate, but not everyone is a good candidate for a pneumatic retinopexy.
- Scleral buckle. This is a surgery that needs to be performed in the operating room. This procedure involves placing a silicone band around the outside of the eye to bring the eye wall closer to the retina. The retinal tear is then treated with a freezing procedure.
- Vitrectomy. In this surgery, the gel - the vitreous inside the eye - is removed and the fluid underneath the retina is drained. The retinal tear is then treated with either a laser or freezing procedure. At the completion of the surgery, a gas bubble fills the eye to hold the retina in place. The gas bubble will slowly dissipate over several weeks. Sometimes a scleral buckle is combined with a vitrectomy surgery.
Prognosis
The final vision after retinal detachment repair is usually dependent on whether the center of the retina - called the macula - is involved. If the macula is detached, then there is usually some decrease in final vision after reattachment. Therefore, a good predictor is initial presenting vision. We recommend that anyone with symptoms of retinal detachments (flashes, floaters, or field cuts) have a dilated eye exam. The sooner the diagnosis is made, the better the treatment outcome.
Article contributed by Dr. Jane Pan
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Fall brings a lot of fun, with Halloween bringing loads of it.
But did you know that some Halloween practices could harm your vision? Take Halloween contacts, for instance. They vary widely, with everything from monster eyes to goblin eyes to cat eyes to sci-fi or glamour looks. They can be just the added touch you need for that perfect costume. However, some people do not realize that the FDA classifies contact lenses as medical devices that can alter cells of the eye and that damage can occur if they are not fit properly.
Infection, redness, corneal ulcers, hypoxia (lack of oxygen to the eye) and permanent blindness can occur if the proper fit is not ensured. The ICE, FTC, and FDA are concerned about costume contacts from the illegal black market because they are often unsafe and unsanitary. Proper safety regulations are strictly adhered to by conventional contact lens companies to ensure that the contact lenses are sterile and packaged properly and accurately.
Health concerns arise whenever unregulated black-market contacts come into the US market and are sold at flea markets, thrift shops, beauty shops, malls, and convenience stores. These contacts are sold without a prescriber's prescription, and are illegal in the US. There have also been reports of damage to eyes because Halloween spook houses sometimes ask employees to share the same pair of Halloween contact lenses as they dress up for their roles.
So the take home message is, have a great time at Halloween, and enjoy the flare that decorative contacts can bring to your costume, but get them from a reputable venue and be fit by an eye care professional with a proper legal prescription. Don't gamble with your eyes for a night of Halloween fun!
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

The eye holds a unique place in medicine. Your eye doctor can see almost every part of your eye from an exterior view. Other than your skin, almost every other part of your body cannot be fully examined without either entering the body (with a scope) or scanning your body with an imaging device (such as a CAT scan, MRI, or ultrasound).
This gives your eye doctor the ability to find many eye problems just by looking in your eye. Even though that makes diagnosing most problems more straightforward than in other medical specialties, there are still many things you can do to get the most out of your eye exams. Here are the top 7 things you can do to get as much as possible out of your exam.
1) Bring your corrective eyewear with you. Have glasses? Bring them. Have separate pairs for distance and reading? Bring them both. Have contacts? Bring them with you and not just the lenses themselves but the lenses prescription, which is on the box they came in. What we most want to know is the brand, the base curve (BC) and the prescription. If you have both contacts and glasses bring BOTH--even if you hate them. Knowing what you like and hate, can help us prescribe something that you will love.
2) Know your family history of eye diseases. There are several eye diseases that run in families. The big ones are glaucoma, macular degeneration, and retinal detachments. If you have a family history of one of these, it may change a doctor’s recommendations for intervention compared to someone without a family history.
3) Know your medical problems. There are several medical problems that correlate with certain diseases of the eye. Diabetes, hypertension, thyroid disease, multiple sclerosis, and autoimmune diseases all correlate with particular eye problems. Knowing your medical history greatly increases the likelihood of more accurately dealing with your eye problem.
4) Know your medications. Several medications are known to produce specific eye problems. Drugs like steroids, Plaquenil, Gleevac, amiodarone, fingolamide, diuretics and Topamax, to name a few, can create problems in your eye. Knowing you are on certain medications may make it much easier for the doctor to arrive at a diagnosis of your eye condition.
5) Be calm and do your best. There are several tests we do that require your participation. The two tests that make people most anxious are the refraction (which determines glasses or contacts prescriptions) and a visual field test (which tests your peripheral vision.) Stay calm and give your best answers. There are no perfect answers. You are not going to get shocked for a wrong answer, so don’t ramp up the anxiety. Just give it your best try.
6) Bring someone with you when possible. There are two reasons for this. One is that it is better to not drive home if you are having your eyes dilated. Many people can do it comfortably, but some can’t. If you are not sure you can drive comfortably with your eyes dilated it is better to have someone with you who can drive home. The second reason is that is always better to have a second pair of ears to hear what the doctor is telling you - especially if the problem is significant. There are many studies that show a person often mishears or misremembers what they have been told, especially if they are anxious. Two pairs of ears are better than one.
7) Write down any questions. It’s very easy to forget to ask something you really wanted to know. You will get your questions answered much better if you have written them down prior to your appointment.
Follow these tips and you will have your best experience possible at your next exam.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Read more: 7 Tips from an Eye Doctor on Getting the Most from Your Exam

Oftentimes, contact lens wearers will skimp on their lens care because some of the solutions are costly and it seems like a good way to save some hard-earned cash. But this is not a good idea.
Cutting corners can result in infections or irritations, and after one or two copays to your eye doctor's office you probably will have spent more than what you saved in a year by cutting corners--plus you have to deal with your discomfort and inability to wear your contact lenses while you are being treated.
The reasons you clean your contacts is to give increased lens comfort, prolong lens oxygen permeability, and to protect your eyes from infection. The reason you have to disinfect your contact lenses is - as nasty as it may sound - that your eyeball and eyelids are covered in essential bacteria that are kept in check by your body’s immune system. When you remove your contact lens at night it is covered in these essential bacteria. If you don't kill them overnight this will allow the bacteria to grow unchecked and then, instead of inserting a freshly cleaned lens, you are inserting a lens covered in more bacteria than your eye is used to and you end up getting an infection.
 Let’s talk about the most widely used type of solution - the multipurpose solution. While this is often the most incorrectly used solution, multipurpose solution is a very safe and effective disinfection method when used properly.
Let’s talk about the most widely used type of solution - the multipurpose solution. While this is often the most incorrectly used solution, multipurpose solution is a very safe and effective disinfection method when used properly.
Many multipurpose solutions advertise themselves as “No Rub.” Just put it in the case and you are done. This is OK to do, but a quick rub with the no-rub solution in the palm of your hand and the opposite hand’s middle or ring finger provide an even better cleaning option. Just the slight roughness of your fingerprint adds a light scrubbing effect that helps improve the removal of surface debris, protein, and mucous better than just letting the lens soak overnight. This rubbing of the lens is especially important for women to remove any cosmetics that are rarely removed by just soaking alone. These few seconds of extra cleaning will make your lenses stay more comfortable longer during their wearing cycle, and help to keep the pores of the lenses open, allowing more oxygen to contact your cornea.
Many name brands and store/warehouse brands of multipurpose solutions exist. All are FDA approved to do the same thing: clean/disinfect/rinse/store your contact lenses. You can't really mess them up unless you try. Remove the lenses, lightly rub them with the multipurpose solution, place your lens into a CLEAN and DRY lens case, and cover the lens with solution to disinfect it. Then let it sit for the number of hours recommended by the manufacturer, generally between 4 to 8 hours, or overnight. Remove the lenses in the morning, rinse with the same multipurpose solution and rinse the lens case out and leave it open to air dry in an area away from your sink and toilet to prevent airborne contaminants from getting into your case as it dries.
The biggest misuse of the multipurpose solution is not changing your case’s solution nightly and just adding more solution to the case each night. We call this “topping off the case.” This is NOT safe because it will lose disinfection power since the old/used solution was busy killing the bacteria and organisms from the night before. Just adding a little fresh solution will eventually allow for the bacteria to take over and you may be adding more bacteria into your eyes than if you never disinfected the lenses to begin with.
Multipurpose solution companies oftentimes will give you a new case when you buy bigger bottles of solution. You should start using the new case with the new bottle of solution. Dont's just stash the case away. There are fungi and other organisms that have been demonstrated to grow from very old lens cases so USE the new case and don't keep it for when you break the old one.
There are many different multipurpose solutions on the market. They aren't cheap and it is tempting to purchase “what is on sale” to save a few dollars. If it does the same thing as the expensive one, then why bother spending the extra? But remember, your contacts are like little sponges that soak up your lens solution. The lens companies don't care if brand A’s solution is compatible with brand B’s or C’s. So over time you can develop a sensitivity to one particular brand of solution, or mixing solutions with the same lens can cause a chemical reaction that occurs because the solutions are not compatible. If you are using the same brand regularly and start having issues your doctor may recommend a solution change to another company that you haven't tried and this may potentially solve your problem. But if you have used several different ones in a few weeks prior to your visit it makes it much harder to determine the cause of your irritation.
The generic/store brands are usually fine products but a grocery store or discount chain doesn’t have a factory that makes their solution for them--they purchase it from a larger supplier. These third-party suppliers can alter their recipe for their multipurpose lens solution and you as the consumer would never know. You could just start finding your contacts are not as comfortable as they used to be and it is actually the unknown generic solution change that is bothering you. Brand name companies like Bausch and Lomb, AMO, and Alcon will rarely make product changes without making consumers aware that they've reformulated the product so if something changes with the reformulated product you have a better chance of knowing it than with a generic solution manufacturer.
Finally, there is a product called saline solution. Saline is extremely inexpensive, generally half to a third the price of multipurpose solutions. This is a product made by many different companies and was the first lens solution ever used. Saline solution was initially used in a heat disinfection system where the lenses were boiled nightly. The boiling of the lens provided the disinfection, not the saline solution. The solution was to just to prevent the lens from drying out while you cooked it. You should NEVER use saline solution as a replacement for multipurpose solution. Saline solution is NOT a disinfectant for your lenses. It doesn’t contain an agent that will prevent bacteria and organisms from growing in the case overnight. However, it’s totally acceptable if you want to rinse your lenses in the morning with saline prior to inserting them after they were disinfected with your multipurpose solution.
Oftentimes, a practitioner will recommend a certain type of solution to help with things like dryness, environmental allergies, or allergies to specific solutions. I always recommend to check with your practitioner before making any changes to your lens care solution or lens care routine. The best advice for saving money on your preferred solution is buy extra when it is on sale, buy in bulk, and buy what is most comfortable in a multipurpose solution for you. Then stick with it and use it correctly for many years of happy lens wear.
Article contributed by Dr. Jonathan Gerard
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
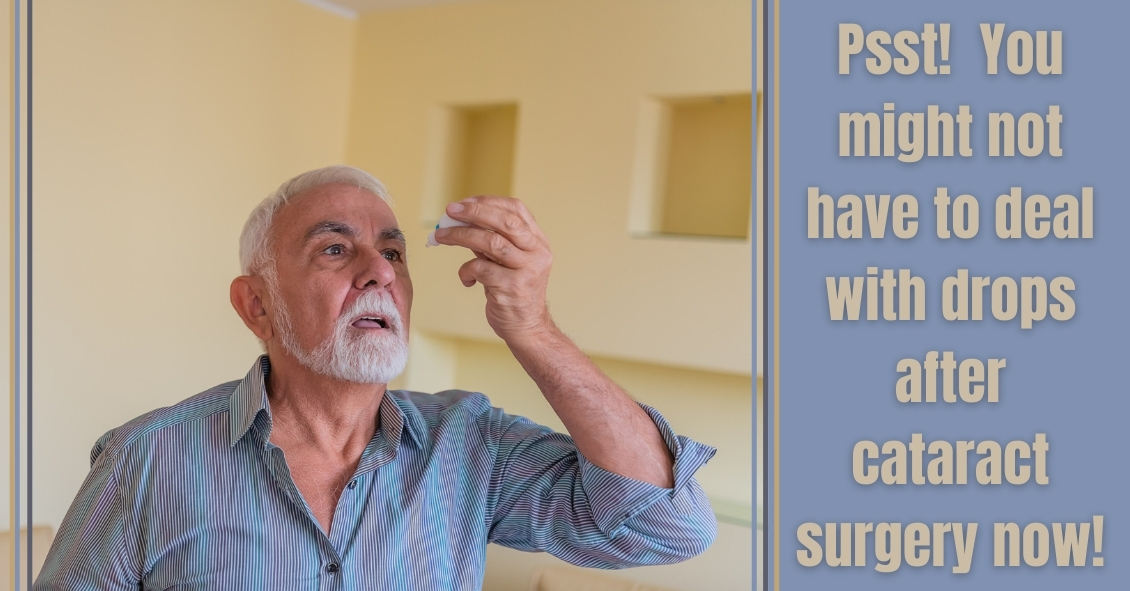
After cataract surgery, there are two main issues we try to control: preventing infection and controlling inflammation. Traditionally, we prescribed antibiotic eye drops to prevent infection, as well as steroid eye drops to control post-operative inflammation. But eye drops can be hard for some patients to put into their eyes. Now we have some alternatives to using drops after surgery.
There are some antibiotic solutions we can place inside the eye at the end of the cataract surgery that have been shown in most studies to do as good or better a job preventing infection as using antibiotic eye drops before and after surgery.
The FDA approved two new steroid delivery methods to reduce post-operative inflammation that have the potential to eliminate post-op steroid eye drops in most (but not all) patients who are undergoing cataract surgery. Those two products are called Dexycu and Dextenza.
Dexycu is a white bolus of steroid medication that is injected inside the eye after cataract surgery. It will not be visible in most patients because it is injected behind the iris, or the colored part of the eye. It sometimes doesn’t stay behind the iris and you might see a small white dot in the eye initially after surgery. It is a sustained-released medication, which is absorbed over a couple of weeks and replaces the need for post-operative steroid drops.
Dextenza is a white pellet that is inserted into the lower punctum of the lid, which is the small opening for the drainage of tears. This insert is designed to deliver medication for up to 30 days. It is slowly absorbed and doesn't need to be removed. Similarly, it is usually not visible and does not cause any discomfort.
If you have either a Dexycu or Dextenza implant placed and an antibiotic medication is injected inside the eye after surgery, then you may be drop free after surgery. The main difference between the two steroid injections is that Dexycu is injected inside the eye while Dextenza is deposited outside the eye. For each of these newer options there is a chance that in your particular case there may still be too much inflammation and you might need to take eye drops for a while, but the majority of the time you would not need drops.
If you are going to have cataract surgery and would like to be drop free after the procedure, then ask your surgeon if you would be a candidate for either the Dexycu or Dextenza implant.
Article contributed by Dr. Jane Pan.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Choosing a new pair of eyeglasses can be a daunting task.
Making a decision on what style glasses you will be wearing for the next year until your vision is checked again can be stressful. This is one of the many reasons opticians are here for you. In many ways, this may be the most important task for the optician, because keeping you happy with the way you look motivates you to wear your glasses daily.
Most people’s reaction is to play it safe with new glasses and stick with something relatively similar to what they are currently wearing.
While not necessarily a bad decision, this isn’t something opticians try to promote. Opticians often spend time meeting with frame representatives and browsing the Internet to keep up with the ever-changing trends in the world of eyeglass frames. And it’s a great feeling to successfully “update” your image with a new set of frames. Many patients are amazed at the difference a well-fit and -styled pair of glasses makes on their overall look.
There are many simple tips and tricks to consider when starting to browse for your next pair of frames.
The goal of this article is to improve your starting point when beginning to choose frames. That way, once the optician gets involved, the process is already well under way. Keep in mind that these are guidelines and “outside the box” thinking can be good as long as it fits within the required parameters of your prescription.
The first step is successfully identifying what face shape category you seem to fit into.
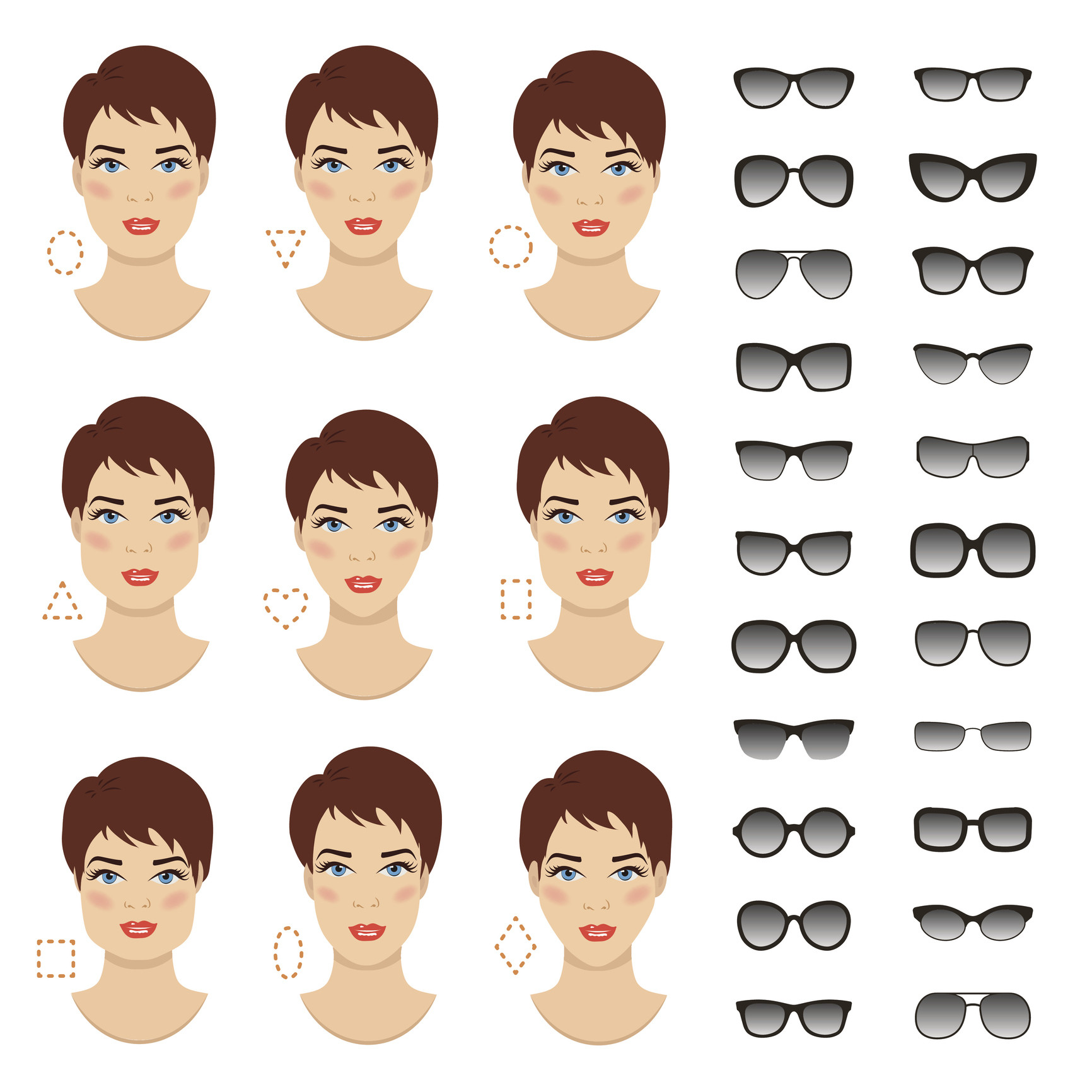 This image shows the most common face-shape categories. The following is a general guideline to help decide which frames will most likely appear to fit the best.
This image shows the most common face-shape categories. The following is a general guideline to help decide which frames will most likely appear to fit the best.
Oval - Oval faces are considered to be the “most versatile” because most frame styles and sizes fit well on this face type. As a general rule, and especially for oval faces, avoid choosing frames that extend past the widest part of your face. Stick with moderate-sized frames.
Upside Down Triangle - To even out the proportions of this face shape, choosing semi-rimless frames is always a positive. Less attention to the bottom half of the frame helps enhance the natural curves of this face shape. Frames that stay wide at the bottom and do not taper inward will also help even out this face.
Oblong - Being longer than it is wide, this face shape enjoys having larger frames on it. A lower bridge will help shorten the nose, and solid dark colors are a positive as well.
Square - A strong jaw line is the focus of this face shape, so to work with that, choosing smaller, narrow frames is a positive. Ovals and rounds work better than squares.
Diamond - Broad cheekbones are the focal point of this face shape. Being quite rare, the best style of frames to put on these faces are in the cat eye family. Following the face’s contours, flare-top frames, semi-rimless frames, and fun colors tend to work well with this shape.
Round - Rectangular frames work best on round faces. Wide bridges help separate the eyes and bring symmetry to the face. Make sure the frames are wider than they are deep.
Triangle - Cat eye frames work exceptionally well with this face shape also. Frames that have a lot of style and accents to the upper part of the frames and temples are a plus as this brings attention to the naturally narrow forehead.
Along with shapes and styles, some believe that certain colors work best with certain faces.
All people are considered to have either cool (blue) or warm (yellow) skin tones. Some people feel customers should stick within their family of coloring. Again this is only a recommendation since you should wear what you like. This is just strictly a guideline for those struggling to choose a frame for themselves. Based on experience, eye color can make a difference as well. People with lighter eyes tend to prefer lighter frame colors, and vice versa for people with darker eyes. Also, hair color can be considered. Patients with lighter or grey hair tend to shy away from darker frames unless looking to make a statement.
At the end of the day you have to choose what is most comfortable for you. Opticians’ suggestions and educated opinions can help steer you in the right direction. There is much to consider, but always keep in mind that comfort and functionality are the priorities.
Some people believe plastic or zyl frames are more comfortable than metal or semi-rimless. Having nose pads, metal frames feel “heavy” to some. Others cannot wear plastic due to oily skin. Plastic frames may slide as the day progresses so metal may be better suited.
Don’t be overwhelmed. Follow some simple guidelines, and remember to enjoy the process. There are infinite styles and options to get you seeing well and looking great. And while you’re considering lenses for your regular lenses, don’t forget to look for sunglasses frames!
Article contributed by Richard Striffolino Jr.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Don't be one of the thousands of parents every year who think, "I wish I had realized sooner that my child coudn't see properly!"
Did you know that early intervention in children's vision is the key to success?
- 80% of learning comes through vision.
- During the first year of life, and then again by age 3 or 4, each child needs a comprehensive eye exam.
- 6 months old is not too early.
Even though a school vision screening, nurse evaluation, or pediatrician screening is important, it doesn't take the place of a comprehensive eye exam by an eyecare professional. Some symptoms of an undetected vision problem include: decreased performance in school, aversion to reading, excessive blinking, eye rubbing, headache, or inability to see 3-D movies properly.
This could indicate conditions such as amblyopia (lazy eye), nearsightedness (myopia), astigmatism, or farsightedness (hyperopia) that can be corrected with glasses.
Surger might even be required for more serious conditions, such as esotropia, where the eye turns in, or exotropia where the eye turns out.
Although school screenings, nurses, and pediatricians are extremely valuable, they don't take the place of a comprehensive eye exam by an optometrist or ophthalmologist.
In fact, school screenings can give a false sense of security. There are visual skills necessary for reading that aren't diagnosed easily just by reading an eye chart. If a child frequently lose his or her place while reading, he or she may benefit from glasses, vision exercises, or therapy.
Vision Therapy involved training the eyes and brain to help alleviate issues that glasses alone can not.
A comprehensive exam can also reveal more serious threats to vision and health in children. A more rare, but life threatening condition is a fast growing eye tumor called retinoblastoma. The proximity of the eye to the brain makes fast intervention critical. This is a condition that parents might notice by looking at pictures and noticing a "white pupil."
Here are some resources to find out more information on children's vision--
- Your local eye care provider.
- Websites such as American Optometric Association.
- The InfantSEE program. It is a no cost public health program for early detection of optical issues in the first year of life.
- Don't Shake is the National center on Shaken Baby Syndrome
- American Academy of Pediatrics
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

