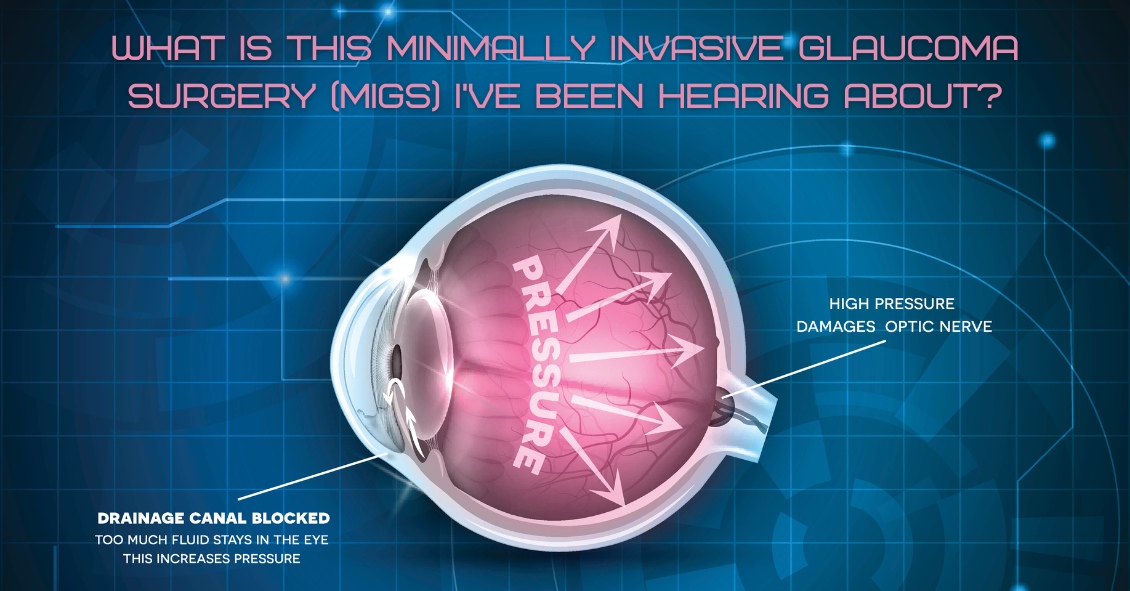
For over 40 years the standard surgical treatment for glaucoma was a procedure called a trabeculectomy.
In a trabeculectomy, the ophthalmic surgeon would make a hole in the wall of eye to allow fluid from the inside of the eye to flow out of the eye and then get resorbed by the blood vessels in the conjunctiva (the mucous membrane that covers the white part of the eye).
This surgery often resulted in a large decrease in the Intraocular Pressure (IOP). Reducing the IOP is the goal of glaucoma surgery because multiple studies show that if you can reduce the pressure the progression of glaucoma slows.
The problem with trabeculectomy is that although it frequently lowers the pressure, it also has a fairly high complication and/or failure rate. This led to some reluctance to perform the procedure unless the glaucoma was severe, or the pressure was very high. As a result of those issues there has been a search during the last 40 years for something that had a lower complication rate and could be more easily deployed earlier in the disease process.
Enter Minimally Invasive Glaucoma Surgery, or MIGS. There are now several types of surgeries that fit in the MIGS category and many of them are used in conjunction with cataract surgery. They are utilized much earlier in the disease process and when combined with cataract surgery they can be used to not only help control the pressure over the long term but can often even reduce the burden of eye drops afterward.
The biggest advantage to MIGS over the trabeculectomy is that when used in conjunction with cataract surgery, MIGS can lower the eye pressure (although not as much as the trabeculectomy) but often with no higher rate of complications as there is with cataract surgery alone.
The lower complication rate is mainly because the MIGS procedures do not create a full-thickness hole in the wall of the eye. Most of them involve putting in some form of stent inside the eye. The stent lets the intraocular fluid get out of the eye more efficiently through its normal internal drain called the trabecular meshwork, rather than having to flow to the outside of the eye as with a trabeculectomy.
A stent is not the only way to lower the pressure along with cataract surgery. There is also a laser treatment you can do from the inside of the eye that slows the amount of fluid the eye makes, which also results in a lower pressure. It is called Endocyclophotocoagulation (ECP). Think of a partially clogged drain in a sink with constantly running water. If you don’t want the sink to overflow (or the pressure in the eye to get too high) you either try to unclog the drain (stent) or you turn down the faucet (ECP).
MIGS has been a great development over the last several years, enabling the surgeon to intervene at a much earlier stage of glaucoma and with a significantly lower complication rate than the more invasive trabeculectomy.
At this point I utilize one of the MIGS procedures in almost all patients who need their cataracts removed and are on one or more glaucoma medications. Even if the glaucoma is fairly well controlled at the time, the MIGS procedure gives us the opportunity to try and get a glaucoma patient off their eye drops, which is both a decreased burden of treatment and lets us keep the eye drops in reserve should the pressure start to increase again later in life.
If you have glaucoma and a cataract you should definitely discuss this with your doctor to see if a MIGS procedure along with your cataract surgery could be the right choice for you.
Article contributed by Dr. Brian Wnorowski, M.D.

What’s up with people wearing those big sunglasses after cataract surgery?
The main reason is for protection - physical protection to assure nothing hits the eye immediately after surgery, and protection from sunlight and other bright lights.
We want to protect the eye from getting hit physically because there is a small incision in the eyeball through which the surgeon has removed the cataract and inserted a new clear lens. In most modern cataract surgeries that incision is very small - about one-tenth of an inch in most cases. The vast majority of surgeons do not stitch the incision closed at the end of surgery. The incision is made with a bevel or flap so that the internal eye pressure pushes the incision closed.
The incision does have some risk of opening, especially if you were to provide direct pressure on the eyeball. Therefore, immediately after surgery we want you to be careful and make sure that you or any outside force doesn’t put direct pressure on the eye. The sunglasses help make sure that doesn’t happen while you are outside immediately after surgery. It’s the same reason that most surgeons ask you to wear a protective plastic shield over the eye at night while you are sleeping for the first week so that you don’t inadvertently rub the eye or smash it into your pillow.
The other advantage of wearing the sunglasses is to protect your eye from bright light, especially in the first day or two when your pupil may still be fairly dilated from all the dilating drops we used prior to surgery. Even after the dilation wears off, the light still seems much brighter than before your surgery. The cataracts act like internal sunglasses. The lens gets more and more opaque as the cataract worsens and so it lets less and less light into the eye. Your eye gets used to those decreased light levels and when you have cataract surgery the eye instantly goes from having all the lights dimmed by the cataract to 100% of the light getting through the new clear lens implant. That takes some getting used to and the sunglasses help you adapt early on. Think of this as if you were in a dark cave for a long period of time and then were thrust out into the bright sunlight. It would be pretty uncomfortable. The sunglasses help with that adjustment.
So why do people keep wearing those sunglasses long after their surgery? Mostly because some people really like them. They not only provide sun protection straight on, they also give you protection along the top and sides of the frame, reducing the light that can enter around the frame
If you have a spouse who wants to keep wearing those...let’s call them “inexpensive” and “less than fashionable”...sunglasses, but you’d like them to look better, there is a solution. There are sunglasses called Fitovers that go over top of your regular glasses and still provide top and side protection from the sun but look much better than the “free” ones you got for cataract surgery.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Is making an appointment for a comprehensive eye exam for your children on your back-to-school checklist? It needs to be.
No amount of new clothes, backpacks, or supplies will allow your child to reach their potential in school if they have an undetected vision problem.
The difference between eye exams and vision screenings
An annual exam done by an eye doctor is more focused than a visual screening done at school. School screenings are simply "pass-fail tests" that are often limited to measuring a child’s sight clarity and visual acuity up to a distance of 20 feet. But this can provide a false sense of security.
There are important differences between a screening and a comprehensive eye exam.
Where a screening tests only for visual acuity, comprehensive exams will test for acuity, chronic diseases, color vision, and eye tracking. This means a child may pass a vision screening at school because they are able to see the board, but they may not be able to see the words in the textbook in front of them.
Why back-to-school eye exams matter
Did you know that 1 out of 4 children has an undiagnosed vision problem because changes in their eyesight go unrecognized?
Myopia, or nearsightedness, is a common condition in children and often develops around the ages of 6 or 7. And nearsightedness can change very quickly, especially between the ages of 11 and 13, which means that an eye prescription can change rapidly over a short period of time. That’s why annual checkups are important.
Comprehensive eye exams can detect other eye conditions. Some children may have good distance vision but may struggle when reading up close. This is known as hyperopia or farsightedness. Other eye issues such as strabismus (misaligned eyes), astigmatism, or amblyopia (lazy eye) are also detectable.
Kids may not tell you they're having visions issues because they might not even realize it. They may simply think everyone sees the same way they do. Kids often give indirect clues, such as holding books or device screens close to their face, having problems recalling what they've read, or avoiding reading altogether. Other signs could include a short attention span, frequent headaches, seeing double, rubbing their eyes, or tilting their head to the side.
What to expect at your child's eye exam
Before the exam, explain that eye exams aren’t scary, and can be fun. A kid-friendly eye exam is quick for your child. After we test how he or she sees colors and letters using charts with pictures, shapes, and patterns, we will give you our assessment of your child’s eyes.
If your child needs to wear glasses, we can even recommend frames and lenses that would be best for their needs.
Set your child up for success
Staying consistent with eye exams is important because it can help your kids see their best in the classroom and when playing sports. Better vision can also mean better confidence because they are able to see well.
Because learning is so visual, making an eye examination a priority every year is an important investment you can make in your child's education. You should also be aware that your health insurance might cover pediatric eye exams.
Set your child up for success and schedule an exam today!
Read more: This Might Just Be the Most Important Test Your Child Will Take

Have you ever heard of Charles Bonnet? He was a Swiss naturalist, philosopher, and biologist (1720-1793) who first described the hallucinatory experiences of his 89-year-old grandfather, who was nearly blind in both eyes from cataracts. Charles Bonnet Syndrome is now the term used to describe simple or complex hallucinations in people who have impaired vision.
Symptoms
People who experience these hallucinations know they aren't real. These hallucinations are only visual, and they don't involve any other senses. These images can be simple patterns or more complex, like faces or cartoons. They are more common in people who have retinal conditions that impair their vision, like macular degeneration, but they can occur with any condition that damages the visual pathway. The prevalence of Charles Bonnet Syndrome among adults 65 years and older with significant vision loss is reported to be between 10% and 40%. This condition is probably under reported because people may be worried about being labeled as having a psychiatric condition.
Causes
The causes of these hallucinations are controversial, but the most supported theory is deafferentation, which in this case is the loss of signals from the eye to the brain; then, in turn, the visual areas of the brain discharge neural signals to create images to fill the void. This is similar to the phantom limb syndrome, when a person feels pain where a limb was once present. In general, the images that are produced by the brain are usually pleasant and non-threatening.
Treatment and prognosis
If there is a reversible cause of decreased vision, such as significant cataract, then once the decreased vision is treated, the hallucinations should stop.
There is no proven treatment for the hallucinations as a result of permanent vision loss but there are some techniques to manage the condition. Give these a try if you have Charles Bonnet Syndrome.
- Talking about the hallucinations and understanding that it is not due to mental illness can be reassuring.
- Changing the environment or lighting conditions. If you are in a dimly lit area, then switch on the light and vice versa.
- Blinking and moving your eyes to the left and right and looking around without moving your head have been reported as helpful.
- Resting and relaxing. The hallucinations may be worse if you are tired or sick.
- Taking antidepressants and anticonvulsants have been used but have questionable efficacy.
Over time, the hallucinations become more manageable and can decrease or even stop after a couple of years.
If you experience any of these symptoms, please get evaluated by your eye doctor to make sure there is not a treatable eye condition. Don’t be embarrassed or ashamed—your issue is likely caused by a physical disturbance and we are here to help!
Article contributed by Jane Pan
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Read more: Charles Bonnet Syndrome and Visual Hallucinations

Fireworks Eye Injuries Have Skyrocketed in Recent Years
Fireworks sales are exploding across the country through the Fourth of July. As retailers are blazing their promotions, we and the AAO are shining a light on this explosive fact--the number of eye injuries caused by fireworks has rocketed in recent years.
Fireworks injuries cause approximately 15,600 emergency room visits each year, according to data from the U.S. Consumer Product Safety Commission. The injuries largely occurred in the weeks before and after the Fourth of July. The CPSC’s fireworks report showed that about 2,340 eye injuries related to fireworks were treated in U.S. emergency rooms in 2020, up from 600 reported in 2011.
To help prevent these injuries, the Academy has addressed four important things about consumer fireworks risks:
- Small doesn’t equal safe. A common culprit of injuries are the fireworks often handed to small children – the classic sparkler. Many people mistakenly believe sparklers are harmless due to their size and the fact they don’t explode. However, they can reach temperatures of up to 2,000 degrees – hot enough to melt certain metals.
- Even though it looks like a dud, it may not act like one. At age 16, Jameson Lamb was hit square in the eye with a Roman candle that he thought had been extinguished. By age 20, Lamb had gone through multiple surgeries, including a corneal transplant and a stem cell transplant to try to restore partial vision to the eye.
- Just because you’re not lighting or throwing it doesn’t mean you’re out of the firing line. An international study of fireworks-related eye injuries showed that half of those hurt were bystanders. The researchers also found that one in six of these injuries caused severe vision loss.
- The Fourth can be complete without using consumer fireworks. The Academy advises that the safest way to view fireworks is to watch a professional show where experts are controlling the displays.
If you experience a fireworks eye injury:
- Seek medical attention immediately.
- Avoid rubbing or rinsing the eyes or applying pressure.
- Do not remove any object from the eye, apply ointments, or take any pain medications before seeking medical help.
Watch the AAO’s animated public service announcement titled “Fireworks: The Blinding Truth.”
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Dry Eye Disease affects more than 5 million people in the United States, with 3.3 million being women and most of those being age 50 or over. And as people live longer, dry eye will continue to be a growing problem.
Although treatment options for dry eyes have improved recently, one of the most effective treatments is avoidance of dry eye triggers.
For some that might mean protecting your eyes from environmental triggers. To do that experts recommend using a humidifier in your home, especially if you have forced hot-air heat; wearing sunglasses when outside to help protect your eyes from the sun and wind that may make your tears evaporate faster; or being sure to direct any fans - such as the air vents in your car - from blowing directly on your face. For others, it may mean avoiding medications that can cause dry eyes.
There is one other trigger that may need to be avoided that doesn’t get as much notice: the potentially harmful ingredients in cosmetics.
Cosmetics do not need to prove that they are “safe and effective” like drugs do. The FDA states that cosmetics are supposed to be tested for safety but there is no requirement that companies share their safety data with the FDA. There are also no specific definition requirements for labeling cosmetics as “hypoallergenic,” “dermatologist tested,” “ophthalmologist tested,” “sensitive formula” or the like, making most of those labels more marketing than science.
Things to watch out for in your cosmetics if you have dry eye include:
Preservatives
Preservatives are important to prevent the cosmetics from becoming contaminated but many are known to exacerbate dry eye. Common preservatives in cosmetics that could be adding to your dry eye problems (Periman and O’Dell, Ophthalmology Management August 2016) are: BAK (Benzalkonium chloride); Formaldehyde-donating (yes, Formaldehyde!) preservatives (often listed as DMDM-hydantoin, quaternium-15, imidazolidinyl urea, diazolidinyl urea and 2-bromo-2-nitropropane-1,3-diol); parabens; and Phenoxyethanol. All of these preservatives in sufficient quantities can cause ocular irritation or inhibit the function of the Meibomian Glands that produce mucous that coats your tear film and keeps it from evaporating too quickly.
Alcohol
Alcohol is used in cosmetics mostly to speed the drying time but the alcohol can also dry the surface of the eye.
Waxes
Waxes can block the opening of the Meibomian Glands along the eyelid margin. If these glands are blocked they will not be able to supply the mucous and lipids necessary to the tear film to prevent it from drying too quickly. If you have trouble with dry eye it would be advisable not to apply eye liner behind the eyelashes along the lid edge where the Meibomian gland openings are.
Anti-aging products
While these may be safe and effective for the skin of the face they should not be used around the eyes. Most of these products contain some form of Retin A. These products have been shown to be toxic to the Meibomian glands and could be contributing to your dry eyes.
These components of cosmetics do not adversely affect everyone. However, if you suffer from dry eye and are not effectively able to keep your eye comfortable and your vision clear, you should investigate your cosmetics as a potential contributor to your problem.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
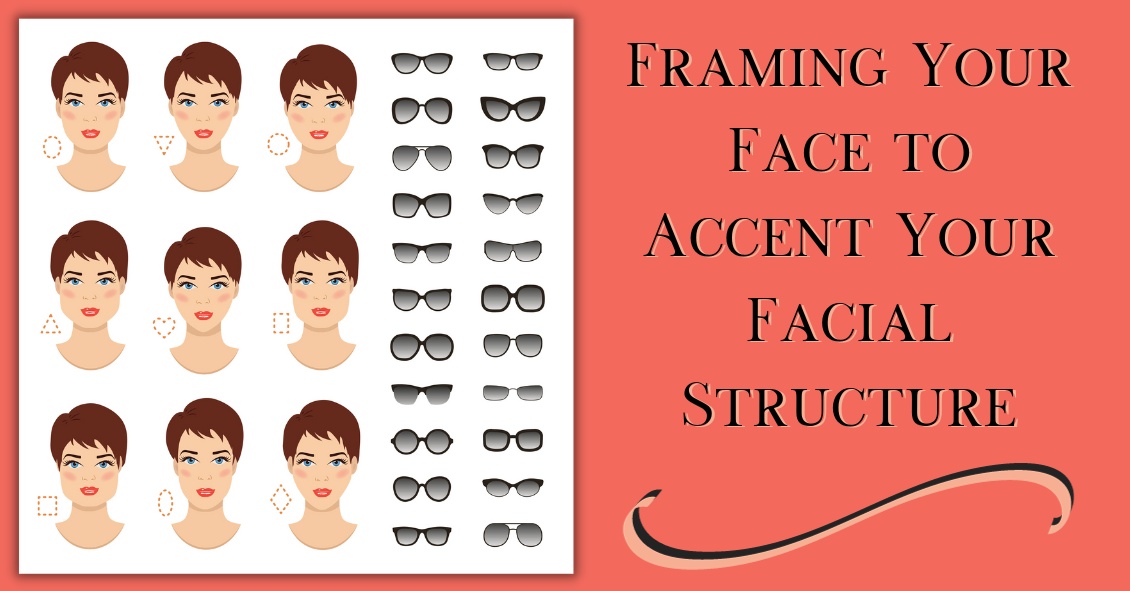
Choosing a new pair of eyeglasses can be a daunting task.
Making a decision on what style glasses you will be wearing for the next year until your vision is checked again can be stressful. This is one of the many reasons opticians are here for you. In many ways, this may be the most important task for the optician, because keeping you happy with the way you look motivates you to wear your glasses daily.
Most people’s reaction is to play it safe with new glasses and stick with something relatively similar to what they are currently wearing.
While not necessarily a bad decision, this isn’t something opticians try to promote. Opticians often spend time meeting with frame representatives and browsing the Internet to keep up with the ever-changing trends in the world of eyeglass frames. And it’s a great feeling to successfully “update” your image with a new set of frames. Many patients are amazed at the difference a well-fit and -styled pair of glasses makes on their overall look.
There are many simple tips and tricks to consider when starting to browse for your next pair of frames.
The goal of this article is to improve your starting point when beginning to choose frames. That way, once the optician gets involved, the process is already well under way. Keep in mind that these are guidelines and “outside the box” thinking can be good as long as it fits within the required parameters of your prescription.
The first step is successfully identifying what face shape category you seem to fit into.
This image shows the most common face-shape categories. The following is a general guideline to help decide which frames will most likely appear to fit the best.
Oval - Oval faces are considered to be the “most versatile” because most frame styles and sizes fit well on this face type. As a general rule, and especially for oval faces, avoid choosing frames that extend past the widest part of your face. Stick with moderate-sized frames.
Upside Down Triangle - To even out the proportions of this face shape, choosing semi-rimless frames is always a positive. Less attention to the bottom half of the frame helps enhance the natural curves of this face shape. Frames that stay wide at the bottom and do not taper inward will also help even out this face.
Oblong - Being longer than it is wide, this face shape enjoys having larger frames on it. A lower bridge will help shorten the nose, and solid dark colors are a positive as well.
Square - A strong jaw line is the focus of this face shape, so to work with that, choosing smaller, narrow frames is a positive. Ovals and rounds work better than squares.
Diamond - Broad cheekbones are the focal point of this face shape. Being quite rare, the best style of frames to put on these faces are in the cat eye family. Following the face’s contours, flare-top frames, semi-rimless frames, and fun colors tend to work well with this shape.
Round - Rectangular frames work best on round faces. Wide bridges help separate the eyes and bring symmetry to the face. Make sure the frames are wider than they are deep.
Triangle - Cat eye frames work exceptionally well with this face shape also. Frames that have a lot of style and accents to the upper part of the frames and temples are a plus as this brings attention to the naturally narrow forehead.
Along with shapes and styles, some believe that certain colors work best with certain faces.
All people are considered to have either cool (blue) or warm (yellow) skin tones. Some people feel customers should stick within their family of coloring. Again this is only a recommendation since you should wear what you like. This is just strictly a guideline for those struggling to choose a frame for themselves. Based on experience, eye color can make a difference as well. People with lighter eyes tend to prefer lighter frame colors, and vice versa for people with darker eyes. Also, hair color can be considered. Patients with lighter or grey hair tend to shy away from darker frames unless looking to make a statement.
At the end of the day you have to choose what is most comfortable for you. Opticians’ suggestions and educated opinions can help steer you in the right direction. There is much to consider, but always keep in mind that comfort and functionality are the priorities.
Some people believe plastic or zyl frames are more comfortable than metal or semi-rimless. Having nose pads, metal frames feel “heavy” to some. Others cannot wear plastic due to oily skin. Plastic frames may slide as the day progresses so metal may be better suited.
Don’t be overwhelmed. Follow some simple guidelines, and remember to enjoy the process. There are infinite styles and options to get you seeing well and looking great. And while you’re considering lenses for your regular lenses, don’t forget to look for sunglasses frames!
Article contributed by Richard Striffolino Jr.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

It's pretty common for eye doctors to have older patients come in asking if the white part of their eye, the sclera, has a growth or is turning a gray color.
Usually, the culprit is senile scleral plaque, which is commonly seen in people over the age of 70. It is a benign condition and more commonly seen in women. This condition is symmetrically found on both sides of the eye and is due to age-related degeneration and calcification of the eye muscle insertion into the eye. In one study, the size of the senile scleral plaque increased as the person aged and was not associated with any medical conditions. People are asymptomatic, as the plaques do not affect vision and no treatment is needed.
Another commonly asked question is: Why is the colored part of my eye turning white?
The colored part of the eye is the iris, which is covered by a clear layer called the cornea. It is actually the edge of the cornea that attaches to the white part of the eye that becomes grey or whitish colored.
This condition is called arcus senilis, which is seen in over 60% of people over the age of 60 and approximately 100% over the age of 80. There is no visual impairment and no treatment is needed. Sometimes when this condition is seen in younger patients, it may be related to high cholesterol, so a visit to the primary care doctor may be needed.
These are two very commonly encountered conditions that may cause distress for patients because it seems like their eyes are changing colors.
Thankfully, no treatment is needed for these two conditions, as they do not affect vision. But if you notice that your eyes are changing colors, it is always a good idea to talk with your eye doctor about it!
Article contributed by Dr. Jane Pan
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
After cataract surgery, there are two main issues we try to control: preventing infection and controlling inflammation. Traditionally, we prescribed antibiotic eye drops to prevent infection, as well as steroid eye drops to control post-operative inflammation. But eye drops can be hard for some patients to put into their eyes. Now we have some alternatives to using drops after surgery.
There are some antibiotic solutions we can place inside the eye at the end of the cataract surgery that have been shown in most studies to do as good or better a job preventing infection as using antibiotic eye drops before and after surgery.
The FDA approved steroid delivery methods to reduce post-operative inflammation that have the potential to eliminate post-op steroid eye drops in most (but not all) patients who are undergoing cataract surgery. Two of these products are called Dexycu and Dextenza.
Dexycu is a white bolus of steroid medication that is injected inside the eye after cataract surgery. It will not be visible in most patients because it is injected behind the iris, or the colored part of the eye. It sometimes doesn’t stay behind the iris and you might see a small white dot in the eye initially after surgery. It is a sustained-released medication, which is absorbed over a couple of weeks and replaces the need for post-operative steroid drops.
Dextenza is a white pellet that is inserted into the lower punctum of the lid, which is the small opening for the drainage of tears. This insert is designed to deliver medication for up to 30 days. It is slowly absorbed and doesn't need to be removed. Similarly, it is usually not visible and does not cause any discomfort.
If you have either a Dexycu or Dextenza implant placed and an antibiotic medication is injected inside the eye after surgery, then you may be drop free after surgery. The main difference between the two steroid injections is that Dexycu is injected inside the eye while Dextenza is deposited outside the eye. For each of these newer options there is a chance that in your particular case there may still be too much inflammation and you might need to take eye drops for a while, but the majority of the time you would not need drops.
If you are going to have cataract surgery and would like to be drop free after the procedure, then ask your surgeon if you would be a candidate for a steroid implant.
Article contributed by Dr. Jane Pan.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Oftentimes, contact lens wearers will skimp on their lens care because some of the solutions are costly and it seems like a good way to save some hard-earned cash. But this is not a good idea.
Cutting corners can result in infections or irritations, and after one or two copays to your eye doctor's office you probably will have spent more than what you saved in a year by cutting corners--plus you have to deal with your discomfort and inability to wear your contact lenses while you are being treated.
The reasons you clean your contacts is to give increased lens comfort, prolong lens oxygen permeability, and to protect your eyes from infection. The reason you have to disinfect your contact lenses is - as nasty as it may sound - that your eyeball and eyelids are covered in essential bacteria that are kept in check by your body’s immune system. When you remove your contact lens at night it is covered in these essential bacteria. If you don't kill them overnight this will allow the bacteria to grow unchecked and then, instead of inserting a freshly cleaned lens, you are inserting a lens covered in more bacteria than your eye is used to and you end up getting an infection.
 Let’s talk about the most widely used type of solution - the multipurpose solution. While this is often the most incorrectly used solution, multipurpose solution is a very safe and effective disinfection method when used properly.
Let’s talk about the most widely used type of solution - the multipurpose solution. While this is often the most incorrectly used solution, multipurpose solution is a very safe and effective disinfection method when used properly.
Many multipurpose solutions advertise themselves as “No Rub.” Just put it in the case and you are done. This is OK to do, but a quick rub with the no-rub solution in the palm of your hand and the opposite hand’s middle or ring finger provide an even better cleaning option. Just the slight roughness of your fingerprint adds a light scrubbing effect that helps improve the removal of surface debris, protein, and mucous better than just letting the lens soak overnight. This rubbing of the lens is especially important for women to remove any cosmetics that are rarely removed by just soaking alone. These few seconds of extra cleaning will make your lenses stay more comfortable longer during their wearing cycle, and help to keep the pores of the lenses open, allowing more oxygen to contact your cornea.
Many name brands and store/warehouse brands of multipurpose solutions exist. All are FDA approved to do the same thing: clean/disinfect/rinse/store your contact lenses. You can't really mess them up unless you try. Remove the lenses, lightly rub them with the multipurpose solution, place your lens into a CLEAN and DRY lens case, and cover the lens with solution to disinfect it. Then let it sit for the number of hours recommended by the manufacturer, generally between 4 to 8 hours, or overnight. Remove the lenses in the morning, rinse with the same multipurpose solution and rinse the lens case out and leave it open to air dry in an area away from your sink and toilet to prevent airborne contaminants from getting into your case as it dries.
The biggest misuse of the multipurpose solution is not changing your case’s solution nightly and just adding more solution to the case each night. We call this “topping off the case.” This is NOT safe because it will lose disinfection power since the old/used solution was busy killing the bacteria and organisms from the night before. Just adding a little fresh solution will eventually allow for the bacteria to take over and you may be adding more bacteria into your eyes than if you never disinfected the lenses to begin with.
Multipurpose solution companies oftentimes will give you a new case when you buy bigger bottles of solution. You should start using the new case with the new bottle of solution. Dont's just stash the case away. There are fungi and other organisms that have been demonstrated to grow from very old lens cases so USE the new case and don't keep it for when you break the old one.
There are many different multipurpose solutions on the market. They aren't cheap and it is tempting to purchase “what is on sale” to save a few dollars. If it does the same thing as the expensive one, then why bother spending the extra? But remember, your contacts are like little sponges that soak up your lens solution. The lens companies don't care if brand A’s solution is compatible with brand B’s or C’s. So over time you can develop a sensitivity to one particular brand of solution, or mixing solutions with the same lens can cause a chemical reaction that occurs because the solutions are not compatible. If you are using the same brand regularly and start having issues your doctor may recommend a solution change to another company that you haven't tried and this may potentially solve your problem. But if you have used several different ones in a few weeks prior to your visit it makes it much harder to determine the cause of your irritation.
The generic/store brands are usually fine products but a grocery store or discount chain doesn’t have a factory that makes their solution for them--they purchase it from a larger supplier. These third-party suppliers can alter their recipe for their multipurpose lens solution and you as the consumer would never know. You could just start finding your contacts are not as comfortable as they used to be and it is actually the unknown generic solution change that is bothering you. Brand name companies like Bausch and Lomb, AMO, and Alcon will rarely make product changes without making consumers aware that they've reformulated the product, so if something changes with the reformulated product you have a better chance of knowing it than with a generic solution manufacturer.
Finally, there is a product called saline solution. Saline is extremely inexpensive, generally half to a third the price of multipurpose solutions. This is a product made by many different companies and was the first lens solution ever used. Saline solution was initially used in a heat disinfection system where the lenses were boiled nightly. The boiling of the lens provided the disinfection, not the saline solution. The solution was to just to prevent the lens from drying out while you cooked it. You should NEVER use saline solution as a replacement for multipurpose solution. Saline solution is NOT a disinfectant for your lenses. It doesn’t contain an agent that will prevent bacteria and organisms from growing in the case overnight. However, it’s totally acceptable if you want to rinse your lenses in the morning with saline prior to inserting them after they were disinfected with your multipurpose solution.
Oftentimes, a practitioner will recommend a certain type of solution to help with things like dryness, environmental allergies, or allergies to specific solutions. I always recommend to check with your practitioner before making any changes to your lens care solution or lens care routine. The best advice for saving money on your preferred solution is buy extra when it is on sale, buy in bulk, and buy what is most comfortable in a multipurpose solution for you. Then stick with it and use it correctly for many years of happy lens wear.
Article contributed by Dr. Jonathan Gerard
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Sunglasses are more than just a fashion statement - they’re important protection from the hazards of UV light.
If you wear sunglasses mostly for fashion that’s great--just make sure the lenses block UVA and UVB rays.
And if you don’t wear sunglasses, it’s time to start.
Here are your top 6 reasons for wearing sunglasses:
#1--Preventing Skin Cancer
One huge way that sunglasses provide a medical benefit is in the prevention of skin cancer on your eyelids. UV light exposure from the sun is one of the strongest risk factors for the development of skin cancers.
Each year there are more new cases of skin cancer than the combined incidence of cancers of the breast, prostate, lung and colon.
About 90 percent of non-melanoma skin cancers are associated with exposure to ultraviolet (UV) radiation from the sun.
Your eyelids, especially the lower eyelids, are also susceptible to UV light and they do develop skin cancers somewhat frequently.
Many people who now regularly apply sunscreen to help protect them from UV light often don’t get that sunscreen up to the edge of their eyelids because they know the sunscreen is going to make their eyes sting and burn. Unfortunately, that leaves the eyelids unprotected. You can help fix that by wearing sunglasses that block both UVA and UVB rays.
#2--Decreasing Risk For Eye Disease
There is mounting evidence that lifetime exposure to UV light can increase your risk of cataracts and macular degeneration. It also increases your risk of getting growths on the surface of your eye called Pinguecula and Pterygiums. Besides looking unsightly, these growths can interfere with your vision and require surgery to remove them.
#3--Preventing Snow Blindness
Snow reflects UV light and on a sunny day the glare can be intense enough to cause a burn on your cornea--much like what happens when people are exposed to a bright welding arc.
#4--Protection From Wind, Dust, Sand
Many times, when you are spending time outdoors and it is windy, you risk wind-blown particles getting into your eyes. Sunglasses help protect you from that exposure. The wind itself can also make your tears evaporate more quickly, causing the surface of your eye to dry out and become irritated, which in turn causes the eye to tear up again.
#5--Decreasing Headaches
People can get headaches if they are light sensitive and don’t protect their eyes from bright sunlight. You can also bring on a muscle tension headache if you are constantly squinting because the sunlight is too bright.
#6--Clearer Vision When Driving
We have all experienced an episode of driving, coming around a turn, looking directly into the direction of the setting or rising sun, and having difficulty seeing well enough to drive safely. Having sunglasses on whenever you are driving in sunlight helps to prevent those instances. Just a general reduction in the glare and reflections that sunlight causes will make you a better and more comfortable driver.
So it’s time to go out there and find yourself a good pair of sunglasses that you look great in and that protect your health, too.
Your eye-care professional can help recommend sunglasses that are right for your needs.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

The eye holds a unique place in medicine. Your eye doctor can see almost every part of your eye from an exterior view. Other than your skin, almost every other part of your body cannot be fully examined without either entering the body (with a scope) or scanning your body with an imaging device (such as a CAT scan, MRI, or ultrasound).
This gives your eye doctor the ability to find many eye problems just by looking in your eye. Even though that makes diagnosing most problems more straightforward than in other medical specialties, there are still many things you can do to get the most out of your eye exams. Here are the top 7 things you can do to get as much as possible out of your exam.
1) Bring your corrective eyewear with you. Have glasses? Bring them. Have separate pairs for distance and reading? Bring them both. Have contacts? Bring them with you and not just the lenses themselves but the lenses prescription, which is on the box they came in. What we most want to know is the brand, the base curve (BC) and the prescription. If you have both contacts and glasses bring BOTH--even if you hate them. Knowing what you like and hate, can help us prescribe something that you will love.
2) Know your family history of eye diseases. There are several eye diseases that run in families. The big ones are glaucoma, macular degeneration, and retinal detachments. If you have a family history of one of these, it may change a doctor’s recommendations for intervention compared to someone without a family history.
3) Know your medical problems. There are several medical problems that correlate with certain diseases of the eye. Diabetes, hypertension, thyroid disease, multiple sclerosis, and autoimmune diseases all correlate with particular eye problems. Knowing your medical history greatly increases the likelihood of more accurately dealing with your eye problem.
4) Know your medications. Several medications are known to produce specific eye problems. Drugs like steroids, Plaquenil, Gleevac, amiodarone, fingolamide, diuretics and Topamax, to name a few, can create problems in your eye. Knowing you are on certain medications may make it much easier for the doctor to arrive at a diagnosis of your eye condition.
5) Be calm and do your best. There are several tests we do that require your participation. The two tests that make people most anxious are the refraction (which determines glasses or contacts prescriptions) and a visual field test (which tests your peripheral vision.) Stay calm and give your best answers. There are no perfect answers. You are not going to get shocked for a wrong answer, so don’t ramp up the anxiety. Just give it your best try.
6) Bring someone with you when possible. There are two reasons for this. One is that it is better to not drive home if you are having your eyes dilated. Many people can do it comfortably, but some can’t. If you are not sure you can drive comfortably with your eyes dilated it is better to have someone with you who can drive home. The second reason is that is always better to have a second pair of ears to hear what the doctor is telling you - especially if the problem is significant. There are many studies that show a person often mishears or misremembers what they have been told, especially if they are anxious. Two pairs of ears are better than one.
7) Write down any questions. It’s very easy to forget to ask something you really wanted to know. You will get your questions answered much better if you have written them down prior to your appointment.
Follow these tips and you will have your best experience possible at your next exam.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

At some point, you might be the victim of one of these scenarios: You rub your eye really hard, or you walk into something, or you just wake up with a red, painful, swollen eye. However it happened, your eye is red, you’re possibly in pain, and you’re worried.
What do you do next?
Going to the Emergency Room is probably not your best bet.
Your first reaction should be to go see the eye doctor.
There are many causes for a red eye, especially a non-painful red eye. Most are relatively benign and may resolve on their own, even without treatment.
Case in point: Everyone fears the dreaded “pink eye,” which is really just a colloquial term for conjunctivitis, an inflammation or infection of the clear translucent layer (conjunctiva) overlying the white part (sclera) of our eye. Most cases are viral, which is kind of like having a cold in your eye (and we all know there is no cure for the common cold).
Going to the ER likely means you’re going to be prescribed antibiotic drops, which DO NOT treat viral eye infections. Your eye doctor may be able to differentiate if the conjunctivitis is viral or bacterial and you can be treated accordingly.
Another problem with going to the ER for your eye problem is that some Emergency Rooms are not equipped with the same instruments that your eye doctor’s office has, or the ER docs may not be well versed in utilizing the equipment they do have.
The primary instrument that your eye doctor uses to examine your eye is called a slit lamp and the best way to diagnose your red eye is a thorough examination with a slit lamp.
Some eye conditions that cause red eyes require steroid drops for treatment. NO ONE should be prescribing steroids without looking at the eye under a slit lamp. If given a steroid for certain eye conditions that may cause a red eye (such as a Herpes infection), the problem can be made much worse.
Bottom line: If you have an eye problem, see an eye doctor.
Going to the ER with an eye problem can result in long periods of waiting time. Remember, you are there along with people having heart attacks, strokes, bad motor vehicle accidents and the like-- “my eye is red” is not likely to get high priority.
Whenever you have a sudden problem with your eye your first move should be to pick up the phone and call an eye doctor. Most eye doctor offices have an emergency phone number in case these problems arise, and again, if there is no pain or vision loss associated with the red eye, it is likely not an emergency.
Article contributed by Dr. Jonathan Gerard
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

There is an old adage in the eye care industry--Glasses are a necessity, contact lenses are a luxury. Ninety-nine percent of the time this is absolutely true. In the absence of unusual eye disorders or very high prescriptions that don’t allow a person to wear glasses comfortably, contact lenses should only ever be worn if there is a good, sturdy, updated set of prescription glasses available, too. This is due to the fact that there are often emergencies where people cannot wear their contact lenses.
In the 21st century, contact lens technology has gotten to the point where we have drastically cut down on the number of adverse events related to contact lens wear. However, human beings were not meant to wear little pieces of plastic in their eyes. Contact lenses are still considered a foreign body in the eye, and sometimes with foreign bodies, our eyes might feel the need to fight back against the “invader.” As such, issues like red eyes, corneal ulcers, eyelid inflammation, dry eyes, and abnormal blood vessel growth can result from wearing contact lenses.
More often than I would like, I have patients who are longtime contact lens wearers come in, and when I inquire as to the condition of their glasses, they say they don’t own any. My next question is inevitably, “What happens if you get an eye infection and you can’t wear your contacts?” I then see the proverbial light bulb go off in their heads followed by a blank stare. Why? “Because I’ve never had a problem before.” Well, just because you maybe have never been in a car accident before, doesn’t mean you shouldn’t wear your seat belt!
I will therefore repeat the most important takeaway here--Glasses are a necessity, contacts are a luxury. Even if you don’t want to go “all out” and get the most expensive frames or lenses in your glasses, having a reliable pair of glasses is an absolute must for any contact lens wearer.
Article contributed by Dr. Jonathan Gerard
Read more: Why You Shouldn't Try to Get By with Just Contact Lenses

Recent Census Bureau data shows a population of approximately 71 million baby boomers (the generation born from 1946-1964). What does that have to do with low vision you may ask? Approximately 40 million people worldwide have some sort of blindness, and aging increases the incidence of macular degeneration and other vision impairment that qualifies them as “low vision” persons.
Low vision is a condition of the eye in which the vision falls below 20/70 in the better seeing eye. It impairs the recipients, rendering them unable to perform daily tasks that others take for granted. With this rising aging population, the awareness of low vision therapy, diagnosis, and treatments are more widely available.
Low vision treatment can help people recover from decreased visual function due to retinal disease, brain injury, neurological damage, and other causes.
It is not only the elderly population that is affected--approximately 20% of low vision patients are children under the age of 18. Childhood genetic disorders of the eye such as retinitis pigmentosa, albinism, Bests disease, ROP, rod/cone disorders, and glaucoma are among the causes of low vision in the pediatric population.
What can be done to help these millions?
There are eye care practitioners that specialize in low vision, as well as therapists. They train the patient to adjust their current lifestyles to make them more independent and utilize the current salvageable vision they do have. For example, if a person has lost their central vision due to macular degeneration, they can be trained to use their peripheral vision to accommodate for many tasks.
Because patients with low vision cannot be corrected with regular eye glasses, the use of telescopes, magnifiers, computer generated aids, training, biofeedback, and optical magnification devices are among some of the resources available to help. Occupational therapists also employ orientation and mobility assistance to help patients in their daily living skills.
There are many technologies that help to improve vision. One such technology is a bionic eye device that uses a pair of glasses with a camera that transmits video data to an implant in the back of that patients eye (the retina). This device uses technology similar to cochlear implants that stimulate auditory nerve signals to restore hearing. In the same way, visual impulses can be restored by stimulating neurons in the retina, brain, or optic nerve.
Maybe the Bionic Man TV series wasn’t too far out there and can someday be a reality............restoring vision to millions.
For more valuable information on low vision visit:
American Occupational Therapy Association AOTA
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Getting your eyes dilated can be inconvenient – dilation makes your eyes light sensitive, which can make it difficult to read books or use phones and computers for a few 4 hours.
So wouldn’t it be great to have another drop to reverse the effects of dilation?
On Dec. 31, 1990, dapiprazole, under the trade name Rev-Eyes, was approved by the FDA and thought to be the answer to all the post-dilation problems. It was marketed for treatment of medically-induced dilation by stimulating pupillary constriction and restoration of accommodative function for reading.
In clinical practice, dapiprazole took between one to two hours to return pupils to pre-dilation size.
Side effects such as stinging upon instillation, conjunctival hyperemia (redness of eye), headache, and a few instances of ptosis (lid drooping), with a possible additional dollar cost to patients, seemed to lessen dapiprazole’s overall clinical benefit.
Reading ability returned in approximately 43 minutes with dapiprazole vs 66 minutes without the drop (Optom Vis Sci 1994 May; 71(5):319-22). The main complaint that people had after using dapiprazole was the conjunctival hyperemia, which lasted more than three hours. The other issue was that dapiprazole was costly, so some practitioners included an additional charge for the reversal of dilation to offset the cost.
The full adverse reaction profile according to Drugs.com is as follows:
"Adverse Reactions: In controlled studies, the most frequent reaction to dapiprazole was conjunctival injection lasting 20 minutes in over 80% of patients. Burning on instillation of dapiprazole hydrochloride ophthalmic solution was reported in approximately half of all patients. Reactions occurring in 10% to 40% of patients included ptosis, lid erythema, lid edema, chemosis, itching, punctate keratitis, corneal edema, browache, photophobia and headaches. Other reactions reported less frequently included dryness of eyes, tearing and blurring of vision."
Currently, Rev-Eyes is off the market. The FDA has stated that Rev-Eyes was not withdrawn from the market for reasons of safety or effectiveness.
At this time, there is nothing available for reversal of dilation. People who get dilated will still need to wear their sunglasses and to put off reading for a couple of hours until the effects of the dilation drops wear off.
Article contributed by Dr. Jane Pan
This blog provides general information and discussion about eye health and related subjects. The words and other content provided on this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Read more: Why Dilation Reversal Drops Are Not Currently an Option
We are frequently asked if it’s wise to have cataract surgery if you have Macular Degeneration.
Let’s start with some background.
- Cataracts and Age-related Macular Degeneration (AMD) are both leading causes of visual impairment in the elderly population.
- Cataracts develop when the normal clear lens gets cloudy with age. This is correctable with cataract surgery, which involves replacing the cloudy lens with a clear, artificial lens.
- While cataracts affect the front part of the eye, AMD causes damage to the retina, which is the inner back lining of the eye.
There have been concerns about cataract surgery causing progression of AMD. It has been thought that there was an inflammatory component to AMD and the normal inflammatory response after cataract surgery may lead to AMD progression.
But studies have looked at patients who underwent cataract surgery compared to patients who didn't have cataract surgery and the progression of AMD was not significantly different between the two groups. However, those patients with AMD who underwent cataract surgery had a significant improvement in vision.
AMD patients can further be characterized as having wet or dry AMD, and only those with wet AMD require treatment. Patients with wet AMD need injections to decrease the growth of new blood vessels and reduce fluid in the retina.
A 2015 study showed that after cataract surgery, there was an increase in fluid in the retina of patients with wet AMD. Therefore, in patients with wet AMD, we usually want the wet AMD to be stabilized before the patient has cataract surgery. Sometimes an injection may be given prior to cataract surgery to prevent any inflammatory changes that may be associated with cataract surgery.
The majority of the studies on the subject conclude that it is relatively safe to have cataract surgery even if you have AMD and in most cases there is a significant improvement in vision. Removing the cloudy lens also helps the ophthalmologist to better monitor the status of the AMD. You will want to have a candid discussion with your eye doctor on the timing, benefits, and potential risks of cataract surgery with macular degeneration.
Article contributed by Dr. Jan Pan.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Mark your Calendars!!! On Monday, April 8, a solar eclipse will be visible across the entire continental United States and most of Canada.
A solar eclipse occurs when the moon blocks any part of the sun, and with this one, the vast majority of North America will experience at least a partial eclipse.
A lucky few million people along a path from Texas to Kentucy to Ohio to Maine and eastern Canada will experience a brief total eclipse when the moon completely blocks the sun for up to 4 minutes. During this time, it will look like dusk along that path.
This total eclipse will make the solar corona visible, and stars and the planets may also be visible during this time.
But looking directly at the sun before it is completely covered is unsafe. Although there is a limited chance of eye damage if you are in the proper area during the total eclipse it is not worth the risk of retinal damage to even take a quick look at the eclipse if it is not “total.”
A large part of the country is not along the pathway where the eclipse will be total so you should not, and residents should never look at the sun without protection.
The only safe way to look directly at the eclipse is through special solar filters, such as “eclipse glasses” or hand-held solar viewers.
Ordinary sunglasses, even if they are very dark and polarized, are not safe for looking at the sun. You will want to make sure that your eclipse glasses and handheld solar viewers meet the ISO 12312-2 international standard for such products.
Even if you have ISO 12312-2 eclipse glasses, you MUST follow the instructions to keep your eyes safe. Always supervise children using solar filters.
A couple specific instructions are found below, courtesy of NASA’s eclipse website-- https://science.nasa.gov/eclipses/future-eclipses/eclipse-2024/safety/. For complete instructions, read the entire NASA page.
"Except during the brief total phase of a total solar eclipse, when the Moon completely blocks the Sun’s bright face, it is not safe to look directly at the Sun without specialized eye protection for solar viewing.
Viewing any part of the bright Sun through a camera lens, binoculars, or a telescope without a special-purpose solar filter secured over the front of the optics will instantly cause severe eye injury."
A solar eclipse is one of nature’s grandest spectacles. By following these simple rules, you can safely enjoy the view and be rewarded with memories to last a lifetime. An eclipse is a rare and striking phenomenon you won't want to miss, but you must carefully follow safety procedures. Don't let the warnings scare you away from witnessing this singular spectacle! You can experience the eclipse safely, but it is vital that you protect your eyes at all times with the proper solar filters. No matter what recommended technique you use, do not stare continuously at the sun. Take breaks and give your eyes a rest! Do not use sunglasses: they don't offer your eyes sufficient protection. One excellent resource for safe solar eclipse viewing is here: https://science.nasa.gov/eclipses/safety.
The solar eclipse is a spectacular sight but please remember to watch it safely.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided on this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
- Why did the guy try to avoid eye surgery by rubbing ketchup in his eyes? He had heard that Heinz sight was 20/20.
- Patient: “Doc, I get a stabbing pain in my eye every time I take a sip of coffee." Doctor: “Have you tried taking the spoon out of the mug?"
- What do you call a penguin with no eye? A pengun!
- At what elevation is your vision the best? See Level.
- Why don’t optometrists use tape measures? They’re really good at eyeballing it.
- What did the eyeball say to the eyelid? "I wish you wouldn't keep me in the dark!"
- Why did the pirate walk into the bar? He had his patch on the wrong eye.
- Cop: “Let me know if you see the suspect with one eye.” Bystander: “I already saw him run that way, but I was using both my eyes.”
- Man 1: “I stopped seeing my girlfriend two days ago.” Man 2: “Really? What happened?” Man 1: “She accidentally poked me in the eyes.”
- Woman 1: “I used to date a man with a lazy eye.” Woman 2: “Why did you stop?” Woman 1: “He was seeing someone on the side.”
- Patient: “Doc, my eyes are really dry.” Eye Doctor: “Here, smell this onion.” Patient: “That made me cry!” Eye Doctor: “Great, I pulled out the onion to make you moist-your-eyes.”
- How are your eye doctor and your teacher the same? They both spend their days testing pupils!

There are many things that can cause your eye to turn red.
The eye looks red when the blood vessels that are in the conjunctiva (the mucous membrane that covers the white of your eye and the backside of your eyelids) becomes dilated.
Those blood vessels often dilate when the eye gets irritated. This irritation can originate from a problem occurring inside the eye or factors from outside the eye.
The most common external factors that can cause the eye to become red are exposure to infectious organisms (mostly viruses and bacteria), environmental irritants (smoke, chemicals, sunlight), or allergens.
Infectious organisms can cause infectious conjunctivitis, or what is more commonly referred to as “pink eye.” This condition often presents with the eye being red and a mucous discharge being produced, often to such a degree that the eyelids are crusted over upon awaking in the morning. Infectious conjunctivitis can be extremely contagious and it is often advised that you severely limit your exposure to others while the problem is active. Infectious conjunctivitis caused by bacteria can be treated with antibiotic eye drops but viral conjunctivitis currently has no treatment and must run its course like the common cold.
Environmental irritants can make the eye look red for a short period of time during and immediately after exposure. The irritation is usually self-limited but may resolve more quickly with the use of over-the-counter lubricating drops or artificial tears. It is very important to understand exactly which irritant you were exposed to because there are some chemicals (acids and bases) that can cause extreme damage to the eye. So if you’re exposed to a caustic chemical you need to immediately rinse your eye out with water and seek emergency medical attention.
Allergens can cause allergic conjunctivitis, which can look very similar to pink eye but usually has significantly less mucous discharge and is usually accompanied by fairly severe itching. Allergic conjunctivitis is not contagious and can usually be treated with anti-allergy eye drops.
Infectious and allergic conjunctivitis can cause mild discomfort and itching but they rarely cause significant pain or loss of vision. A red eye with significant pain, especially when accompanied by severe light sensitivity and vision loss, often indicates more significant problems such as iritis, angle closure glaucoma or a corneal ulcer, all of which require immediate medical attention. If your eye is red and there is significant pain do not assume you have pink eye--see your eye doctor immediately!
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.