
A common in-office procedure is an eye injection for treatment of various eye conditions, such as wet macular degeneration, diabetic retinopathy, or vein occlusion.
It is normal to be anxious prior to your first eye injection but knowing what to expect may alleviate some anxiety.
Your eye will be numbed with topical anesthetic drops. Usually, a cotton-tipped applicator soaked in anesthetic will be held against the white part of the eye to numb it. Sometimes, a thick gel may also be used for numbing. Once the eye is numbed, it will then be cleaned and a small instrument will be used to hold the eye open. During the actual injection, some patients feel pressure while others may feel a quick sting. Each person will have a different experience and each injection will be different.
The medicine is injected into the white part of the eye. Sometimes a blood vessel may be encountered during the injection and you may notice a little redness on the outside of the eye. This is purely a cosmetic symptom and the redness will disappear within the next couple of days. Patients may also experience some mild irritation after the injection due to the drops that are placed in the eye. I usually recommend over-the-counter artificial tears to use after the injections. Usually, the eye should feel normal by the next day.
Another common symptom after an injection are floaters. These floaters usually appear as small bubbles in the lower half of your vision, but they will disappear in in a day or two.
There are no activity restrictions after the injection and no antibiotic drops are needed.
Things to watch for after the injection:
- If your eye gets painful or redness develops a couple of days after the injection, then you should call your doctor.
- If your vision declines or you notice increased or hundreds of floaters then you should call to be seen.
Otherwise, patients are usually initially seen once a month after they first start injections.
Article contributed by Dr. Jane Pan
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
The retina is the nerve tissue that lines the inside back wall of your eye. Light travels through the pupil and lens and is focused on the retina, where it is converted into a neural impulse and transmitted to the brain. If there is a break in the retina, fluid can track underneath the retina and separate it from the eye wall. Depending on the location and degree of retinal detachment, there can be very serious vision loss.
Symptoms
The three 3 F’s are the most common symptoms of a retinal detachment:
Flashes: Flashing lights that are usually seen in peripheral (side) vision.
Floaters: Hundreds of dark spots that persist in the center of vision.
Field cut: Curtain or shadow that usually starts in peripheral vision that may move to involve the center of vision.
Causes
Retinal detachments can be broadly divided into three categories depending on the cause of the detachment:
Rhegmatogenous retinal detachments: Rhegmatogenous means “arising from a rupture,” so these detachments are due to a break in the retina that allows fluid to collect underneath the retina. A retinal tear can develop when the vitreous (the gel-like substance that fills the back cavity of the eye) separates from the retina as part of the normal aging process.
The risk factors associated with this type of retinal detachment:
Lattice degeneration – thinning of the retina.
High myopia (nearsighted) - can result in thinning of the retina.
History of a previous retinal break or detachment in the other eye.
Trauma.
Family history of retinal detachment.
Tractional retinal detachments: These are caused by scar tissue that grows on the surface of the retina and contraction of the scar tissue pulls the retina off the back of the eye. The most common cause of scar tissue formation is due to uncontrolled diabetes.
Exudative retinal detachments: These types of detachments form when fluid accumulates underneath the retina. This is due to inflammation inside the eye that results in leaking blood vessels. The visual changes can vary depending on your head position because the fluid will shift as you move your head. There is no associated retinal hole or break in this type detachment. Of the three types of retinal detachments, exudative is the least common.
Diagnostic tests
A dilated eye exam is needed to examine the retina and the periphery. This may entail a scleral depression exam where gentle pressure is applied to the eye to examine the peripheral retina.
A scan of the retina (optical coherence tomography) may be performed to detect any subtle fluid that may accumulate under the retina.
If there is significant blood or if a clear view of the retina is not possible for some other reason, then an ultrasound of the eye may be performed.
Treatment
The goal of treatment is to re-attach the retina to the eye wall and to treat the retinal tears or holes.
In general, there are four treatment options:
Laser: A small retinal detachment can be walled off with a barrier laser to prevent further spread of the fluid and the retinal detachment.
Pneumatic Retinopexy: This is an office-based procedure that requires injecting a gas bubble inside the eye. After this procedure, you need to position your head in a certain direction for the gas bubble to reposition the retina back along the inside wall of the eye. A freezing or laser procedure is performed around the retinal break. This procedure has about 70% to 80% success rate but not everyone is a good candidate for a pneumatic retinopexy.
Scleral buckle: This is a surgery that needs to be performed in the operating room. This procedure involves placing a silicone band around the outside of the eye to bring the eye wall closer to the retina. The retinal tear is then treated with a freezing procedure.
Vitrectomy: In this surgery, the vitreous inside the eye is removed and the fluid underneath the retina is drained. The retinal tear is then treated with either a laser or freezing procedure. At the completion of the surgery, a gas bubble fills the eye to hold the retina in place. The gas bubble will slowly dissipate over several weeks. Sometimes a scleral buckle is combined with a vitrectomy surgery.
Prognosis
Final vision after retinal detachment repair is usually dependent on whether the macula (central part of the retina that you use for fine vision) is involved. If the macula is detached, then there is usually some decrease in final vision after reattachment. Therefore, a good predictor is initial presenting vision. We recommend that patients with symptoms of retinal detachments (flashes, floaters, or field cuts) have a dilated eye exam. The sooner the diagnosis is made, the better the treatment outcome.
Article contributed by Dr. Jane Pan
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Read more: What's a retinal detachment and what are the symptoms?
What Is Intraoperative Aberrometry?
Yes, that is a mouthful, but the concept isn’t quite as hard as the name.
An Intraoperative Aberrometer is an instrument we can use in the operating room to help us determine the correct power of the implant we put in your eye during cataract surgery.
Cataract surgery is the removal of the cloudy natural lens of your eye and the insertion of a new artificial lens inside your eye called an intraocular lens (IOL).
The cloudy cataract that we are removing has focusing power (think of a lens in a camera) and when that lens is removed, we need to insert an artificial lens in its place to replace that focusing power. The amount of focusing power the new IOL needs has to match the shape and curvature of your eye.
To determine what power of lens we select to put in your eye, we need to measure the shape and curvature of your eye prior to surgery. Once we get those measurements, we can plug those numbers into several different formulas to try and get the most accurate prediction of what power lens you need.
Overall, those measurements and formulas are very good at accurately predicting what power lens you should have. There are, however, several eye types where those measurements and formulas are less accurate at predicting the proper power of the replacement lens.
Long Eyes: People who are very nearsighted usually have eyes that are much longer than average. This adds some difficulty with the accuracy of both the measurements and the formulas. There are special formulas for long eyes but even those are less accurate than formulas for normal length eyes.
Short Eyes: People who are significantly farsighted tend to have shorter-than-normal eyes. Basically, the same issues hold true for them as the ones for longer eyes noted above.
Eyes with previous refractive surgery (LASIK, PRK, RK): These surgeries all change the normal shape of the cornea. This makes the formulas we use on eyes that have had previous surgery not work as well when the normal shape of the cornea has been altered.
This is where intraoperative aberrometry comes in. The machine takes the measurements that we do before surgery and then remeasures the eye while you are on the operating room table after the cataract is removed and before the new implant is placed inside the eye. It then presents the surgeon with the power of the implant that the aberrometer thinks is the correct one. Unfortunately, the power that the aberrometer selects isn’t always exactly right, but with the combination of the pre-surgery measurements and the intra-surgery measurements the overall accuracy is significantly enhanced.
The intraoperative aberrometry is also very helpful in choosing the power of specialty lenses like multi-focal and toric lenses.
We would encourage you to consider adding intraoperative aberrometry to your cataract surgery procedure if you have either a long or short eye (usually manifested as a high prescription in your glasses) or if you have had any previous refractive surgery.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Read more: What You Should Know About Intraoperative Aberrometry Before Your Cataract Surgery

We all know that during pregnancy, a woman's body goes through a great deal of change hormonally and physiologically. But did you know her eyes change as well? Below are some of the most common effects pregnancy can have on the eye.
- Corneal changes. In some cases, pregnancy can cause the cornea, the front window of the eye, to change curvature and even swell, leading to shifts in glasses and contact lens prescriptions. In addition, changes in the chemistry of the tear film can lead to dry eyes and contact lens intolerance. It is for these reasons that it is generally not recommended to have any new contact lens fitting or new glasses prescription checks until several months postpartum. We want to get the most accurate measurements possible.
- Retinal changes. Many different conditions can affect the retina during pregnancy. If the pregnant woman has diabetes, diabetic eye disease can progress by 50%. In women with preeclampsia, a condition where blood pressure rises significantly, over 40% of women can show changes in the retinal blood vessels, and 25% to 50% complain of changes to their vision.
- Eye Pressure Fluctuation. Intraocular pressure (IOP) usually decreases during pregnancy. The exact mechanism causing this is unknown, but it is usually attributed to an increase of flow of intraocular fluid out of the eye. This is good news for pregnant women with glaucoma or high IOP. In fact, the drop in IOP is larger when you start with a high IOP compared to one in the normal range.
There are many more effects that pregnancy can have on the eye, but these are the most common. One other thing to keep in mind is that though the likelihood of any adverse effect is extremely low, we try not to use any diagnostic eye drops on pregnant patients during the eye exam. Unless there is a medical necessity to dilate the pupils or check IOP, it is a good rule of thumb to put off using drops until after the patient has given birth in order to protect the developing baby.
Article contributed by Dr. Jonathan Gerard
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Recent Census Bureau data shows a population of approximately 70 million baby boomers (the generation born from 1946-1964). What does that have to do with low vision you may ask? Approximately 40 million people worldwide have some sort of blindness, and aging increases the incidence of macular degeneration and other vision impairment that qualifies them as “low vision” persons.
Low vision is a condition of the eye in which the vision falls below 20/70 in the better seeing eye. It impairs the recipients, rendering them unable to perform daily tasks that others take for granted. With this rising aging population, the awareness of low vision therapy, diagnosis, and treatments are more widely available.
Low vision treatment can help people recover from decreased visual function due to retinal disease, brain injury, neurological damage, and other causes.
It is not only the elderly population that is affected--approximately 20% of low vision patients are children under the age of 18. Childhood genetic disorders of the eye such as retinitis pigmentosa, albinism, Bests disease, ROP, rod/cone disorders, and glaucoma are among the causes of low vision in the pediatric population.
What can be done to help these millions?
There are eye care practitioners and therapists that specialize in low vision. They train patients to adjust their current lifestyles to make them more independent and utilize the current salvageable vision they do have. For example, if a person has lost their central vision due to macular degeneration, they can be trained to use their peripheral vision for many tasks.
Because patients with low vision cannot be functionally corrected with regular eye glasses, the use of telescopes, magnifiers, computer generated aids, training, biofeedback, and optical magnification devices are among some of the resources available to help. Occupational therapists also employ orientation and mobility assistance to help patients in their daily living skills.
There are many technologies that help to improve vision. One such technology is a bionic eye device that uses a pair of glasses with a camera that transmits video data to an implant in the back of that patients eye (the retina). This device uses technology similar to cochlear implants that stimulate auditory nerve signals to restore hearing. In the same way, visual impulses can be restored by stimulating neurons in the retina, brain, or optic nerve.
Maybe the Bionic Man TV series wasn’t too far out there and can someday be a reality............restoring vision to millions.
For more valuable information on low vision visit:
American Optometric Association AOA
American Occupational Therapy Association AOTA
American Academy of Ophthalmology AAO
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Age-related macular degeneration, often called ARMD or AMD, is the leading cause of vision loss among Americans 65 and older.
AMD causes damage to the macula, which is the central portion of the retina responsible for sharp central vision. AMD doesn't lead to complete blindness because peripheral vision is still intact, but the loss of central vision can interfere with simple everyday activities such as reading and driving, and it can be very debilitating.
Types of Macular Degeneration
There are two types of macular degeneration: Dry AMD and Wet AMD.
Dry (non-exudative) macular degeneration constitutes approximately 85-90% of all cases of AMD. Dry AMD results from thinning of the macula or the deposition of yellow pigment known as drusen in the macula. There may be gradual loss of central vision with dry AMD, but it is usually not as severe as wet AMD vision loss. However, dry AMD can slowly progress to late-stage geographic atrophy, which can cause severe vision loss.
Wet (exudative) macular degeneration makes up the remaining 10-15% of cases. Exudative or neovascular refers to the growth of new blood vessels in the macula, where they are not normally present. The wet form usually leads to more serious vision loss than the dry form.
AMD Risk factors
- Age is the biggest risk factor. Risk increases with age.
- Smoking. Research shows that smoking increases your risk.
- Family history. People with a family history of AMD are at higher risk.
- Race. AMD is more common in Caucasians than other races, but it exists in every ethnicity.
- Gender. AMD is more common in women than men.
Detection of AMD
There are several tests that are used to detect AMD.
A dilated eye exam can detect AMD. Once the eyes are dilated, the macula can be viewed by the ophthalmologist or optometrist. The presence of drusen and pigmentary changes can then be detected.
An Amsler Grid test uses pattern of straight lines that resemble a checkerboard. It can be used to monitor changes in vision. The onset of AMD can cause the lines on the grid to disappear or appear wavy and distorted.
Fluorescein Angiogram is a test performed in the office. A fluorescent dye is injected into the arm and then a series of pictures are taken as the dye passes through the circulatory system in the back of the eye.
Optical coherence tomography (OCT) is a test based on ultrasound. It is a painless study where high-resolution pictures are taken of the retina.
Article contributed by Jane Pan M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

What Is Intraoperative Aberrometry?
Yes, that is a mouthful, but the concept isn’t quite as hard as the name.
An Intraoperative Aberrometer is an instrument we can use in the operating room to help us determine the correct power of the implant we put in your eye during cataract surgery.
Cataract surgery is the removal of the cloudy natural lens of your eye and the insertion of a new artificial lens inside your eye called an intraocular lens (IOL).
The cloudy cataract that we are removing has focusing power (think of a lens in a camera) and when that lens is removed, we need to insert an artificial lens in its place to replace that focusing power. The amount of focusing power the new IOL needs has to match the shape and curvature of your eye.
To determine what power of lens we select to put in your eye, we need to measure the shape and curvature of your eye prior to surgery. Once we get those measurements, we can plug those numbers into several different formulas to try and get the most accurate prediction of what power lens you need.
Overall, those measurements and formulas are very good at accurately predicting what power lens you should have. There are, however, several eye types where those measurements and formulas are less accurate at predicting the proper power of the replacement lens.
Long Eyes: People who are very nearsighted usually have eyes that are much longer than average. This adds some difficulty with the accuracy of both the measurements and the formulas. There are special formulas for long eyes but even those are less accurate than formulas for normal length eyes.
Short Eyes: People who are significantly farsighted tend to have shorter-than-normal eyes. Basically, the same issues hold true for them as the ones for longer eyes noted above.
Eyes with previous refractive surgery (LASIK, PRK, RK): These surgeries all change the normal shape of the cornea. This makes the formulas we use on eyes that have had previous surgery not work as well when the normal shape of the cornea has been altered.
This is where intraoperative aberrometry comes in. The machine takes the measurements that we do before surgery and then remeasures the eye while you are on the operating room table after the cataract is removed and before the new implant is placed inside the eye. It then presents the surgeon with the power of the implant that the aberrometer thinks is the correct one. Unfortunately, the power that the aberrometer selects isn’t always exactly right, but with the combination of the pre-surgery measurements and the intra-surgery measurements the overall accuracy is significantly enhanced.
The intraoperative aberrometry is also very helpful in choosing the power of specialty lenses like multi-focal and toric lenses.
We would encourage you to consider adding intraoperative aberrometry to your cataract surgery procedure if you have either a long or short eye (usually manifested as a high prescription in your glasses) or if you have had any previous refractive surgery.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Read more: Try saying Intraoperative Aberrometry 3 Times Fast!
Is it safe to use "Redness Relief" eye drops regularly?
The short answer is NO.
Here’s the slightly longer answer.
There are several eye “Redness Relief” products on the over-the-counter market, such as those made by Visine, Clear Eyes, and Bausch & Lomb - as well as generic versions sold by pharmacy chains.
Most commonly, the active ingredient in redness relief drops is either Tetrahydrozoline or Naphazoline. Both of these drugs are in a category called sympathomimetics.
Sympathomimetics, the active ingredient in redness relief drops, work though a process called vasoconstriction, an artificial clamping down of the superficial blood vessels on the eye surface. These blood vessels often dilate in response to an irritation. This increase in blood flow is trying to help repair whatever irritation is affecting the surface of the eye. Clamping down on those vessels by using a vasoconstrictor counteracts the body’s efforts to repair the problem.
The other downside to repetitively using redness relief drops is that after the vasoconstrictor wears off the vessels often dilate to an even larger degree than when the process started. This stimulates you to use the drops again.
All of these drops carry these same two warnings on their labels:
Do not overuse as it may produce increased redness of the eye.
Stop using and ask a doctor if you experience eye pain, changes in vision, continued redness or irritation of the eye, condition worsens or persists for more than 72 hours.
Does anyone read those warnings? Almost never.
These drops are meant to be used for a VERY short duration - one or two days. That’s it!
They are not meant to be used indefinitely and they are certainly not meant to be used daily.
Take a good look at that first warning: MAY PRODUCE INCREASED REDNESS OF THE EYE.
If you are using redness relief drops repetitively you are likely making your eye redness WORSE, not better.
If you have been using redness relief drops daily you need to stop and replace them with an artificial tear or lubricating drop - something that DOES NOT say “gets the red out.”
After you make that switch your eyes are initially going to be red as your blood vessels take time to regain their normal vascular tone without the vasoconstrictor clamping down on them. The lubricating drop will actually help to repair the damage done by exposure to adverse conditions. This will decrease the inflammatory signals that make the vessels dilate. You will actually be doing something helpful to the surface of your eyes instead of just masking everything by artificially clamping down on your vessels and decreasing the flow of oxygen and nutrients to the front surface of your eye.
Using redness relief drops if you wear contacts is an even worse idea. If you put the drop in with your contact in, the contact will hold onto the drug and keep it on your eye surface longer, thus likely increasing the vasoconstriction.
Your cornea has no blood vessels in it and it depends on the blood vessels in the conjunctiva over the whites of the eye to bring in nutrients and oxygen. The other source of oxygen for the cornea is what it gets from diffusion from the atmosphere and that is also cut down by the presence of the contact lens.
The redness relief drop combined with the contact lens are now BOTH reducing the levels of oxygen getting to the cornea. Decreased oxygen to the cornea is one of the biggest risks for contact lens-related infections, including corneal ulcers.
Don’t get me wrong, I’m not condemning redness relief drops if used appropriately for a very short time to soothe the eyes if they have been temporarily exposed to elements that made them irritated. For a day or two redness relief drops are fine. But for long-term use or for use while wearing your contacts they are much more likely to cause problems than to provide any benefits.
Article contributed by Dr. Brian Wnorowski, M.D
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
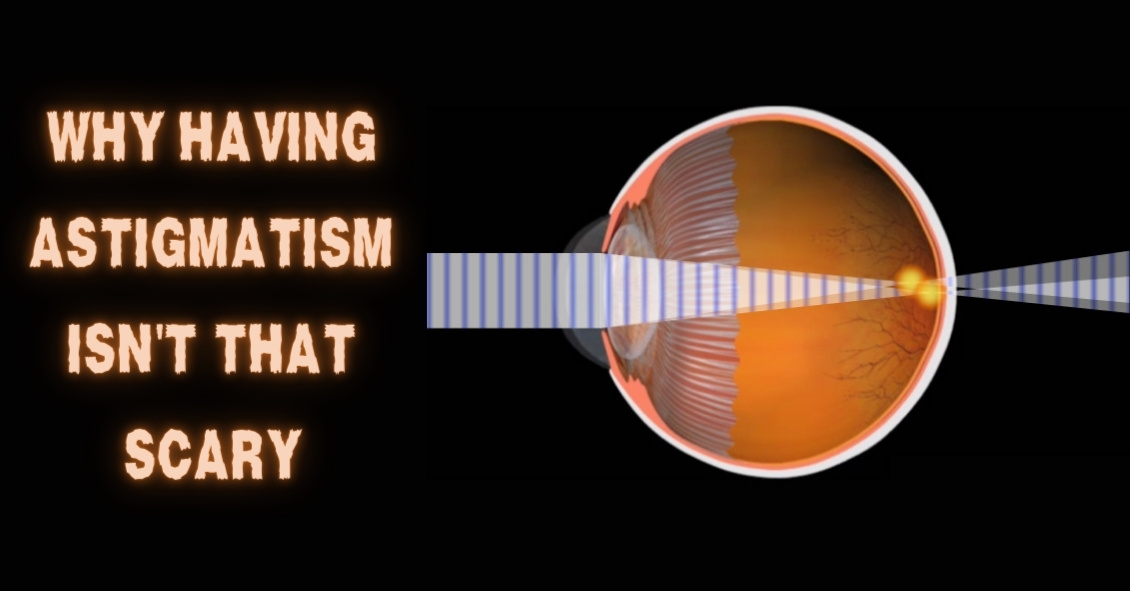
The word “astigmatism” is used so much in the optometric world that most people have talked about it when discussing their eye health with their doctor.
“Astigmatism” comes from the Greek “a” - meaning “without” - and “stigma” - meaning “a point.” In technical ocular terms, astigmatism means that instead of there being one point of focus in the eye, there are two. In other words, light merges not on a single point, but on two different points.
This is experienced in the real world as blurred, hazy vision, and can sometimes lead to eye strain or headaches if not corrected with either glasses or contact lenses.
Astigmatism is not a disease. In fact, more than 90% of people have some degree of astigmatism.
Astigmatism occurs when the cornea, the clear front surface of the eye like a watch crystal, is not perfectly round. The real-world example we often use to explain astigmatism is the difference between a basketball and a football.
If you cut a basketball in half you get a nice round half of a sphere. That is the shape of a cornea without astigmatism.
If you cut a football in half lengthwise you are left with a curved surface that is not perfectly round. It has a steeper curvature on one side and a flatter curve on the other side. This is an exaggerated example of what a cornea with astigmatism looks like.
The degree of astigmatism and the angle at which it occurs is very different from one person to the next. Therefore, two eyeglass prescriptions are rarely the same because there are an infinite number of shapes the eye can take.
Most astigmatism is “regular astigmatism,” where the two different curvatures to the eye lie 90 degrees apart from one another. Some eye diseases or surgeries of the eye can induce “irregular astigmatism,” where the curvatures are in several different places on the eye’s surface, and often the curvatures are vastly different, leading to a high amount of astigmatism.
Regular astigmatism is treated with glasses, contact lenses, or refractive surgery (PRK or LASIK). Irregular astigmatism, such as that caused by the eye disease keratoconus, usually cannot be treated with these conventional methods. In these circumstances, special contact lenses are needed to treat the condition.
The next time you hear that either you or a loved one has astigmatism, fear not.
It is easily corrected, and although astigmatism can cause your vision to be blurry, it rarely causes any permanent damage to the health of your eyes.
If you experience blurred vision, headaches, or eye strain, having a complete eye exam may lead to a diagnosis and treatment of this easily-dealt-with condition.
Article contributed by Dr. Jonathan Gerard
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
There are several different variations of glaucoma, but in this article we will mainly focus on Primary Open Angle Glaucoma. This means that there is no specific underlying cause for the glaucoma, like inflammation, trauma or a severe cataract. It also means that the drainage angle where fluid is drained from the inside of the eye into the bloodstream is not narrow or closed.
Closed or Narrow Angle Glaucoma, which we won't be discussing today, is treated differently from Open Angle Glaucoma
In the U.S., Primary Open Angle Glaucoma (POAG) is by far the most common type of glaucoma we treat.
Glaucoma is a disease where the optic nerve in the back of the eye deteriorates over time, and that deterioration has a relationship to the Intraocular Pressure (IOP). Most - but not all - people diagnosed with glaucoma have an elevated IOP. Some people have fairly normal IOP’s but show the characteristic deterioration in the optic nerve. Regardless of whether or not the pressure was high initially, our primary treatment is to lower the IOP. We usually are looking to try to get the IOP down by about 25% from the pre-treatment levels.
The two mainstays of initial treatment for POAG in the U.S. are medications and laser treatments. There are other places in the world where glaucoma is initially treated with surgery. However, while surgery can often lower the pressure to a greater degree than either medications or laser treatments, it comes with a higher rate of complications. Most U.S. eye doctors elect to go with the more conservative approach and utilize either medications, most often in the form of eye drops, or a laser treatment.
Drops
There are several different classes of medications used to treat glaucoma.
The most common class used are the Prostaglandin Analogues or PGA’s. Some of the PGA’s available in the U.S. are Xalatan (latanaprost), Travatan (travapost), Lumigan (bimatoprost) and Zioptan (tafluprost).
PGA’s are most doctors’ first line of treatment because they generally lower the IOP better than the other classes, they are reasonably well tolerated by most people, and they are dosed just once a day. Most of the other drugs available have to be used multiple times a day.
The other classes of drugs include beta-blockers that are used once or twice a day; carbonic anhydrase inhibitors (CAI’s ), which come in either a drop or pill form and are used either twice or three times a day; alpha agonists that are used either twice or three times a day; and miotics, which are used three or four times a day. All of these other medications are typically used as either second-line or adjunctive treatment when the PGA’s are not successful in keeping the pressure down as single agents.
There are also several combination drops available in the U.S. that combine two of the second-line agents (Cosopt, Combigan, and Symbrinza).
Laser
The second option for initial treatment is a laser procedure.
Two common laser treatments for Open Angle Glaucoma are Argon Laser Trabeculoplasty (ALT) or Selective Laser Trabeculoplasty (SLT). These treatments try to get an area inside the eye called the trabecular meshwork - where fluid is drained from the inside of the eye into the venous system - to drain more efficiently.
These treatments tend to lower the pressure to about the same degree as the PGA’s do with over 80% of patients achieving a significant decrease in their eye pressure that lasts at least a year. Both laser treatments can be repeated if the pressure begins to rise again in the future, but the SLT works slightly better as a repeat procedure compared to the ALT.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Do you have family members with eye-related conditions?
The two main eye diseases in adults that have a genetic link are glaucoma and age-related macular degeneration (AMD).
Glaucoma is a deterioration of the optic nerve caused by pressure in the eye or poor blood flow to the optic nerve. It has no symptoms at its onset. In most cases if you wait to get glaucoma diagnosed until you begin to realize there is something wrong with your vision, upwards of 70% of your optic nerve will have already been destroyed. Once the nerve is destroyed there is no way of reversing that today and treatment is focused on trying to preserve whatever nerve tissue is left.
Your chances of getting glaucoma are four to 10 times higher if you have a close relative with glaucoma. Getting your eyes examined regularly is always important but even more so if there is a family history of glaucoma.
Macular degeneration is the leading cause of blindness in most of the developed world. It too can cause serious vision loss if you wait until you have significant symptoms before a diagnosis. There are now some preventative treatments for AMD--the earlier it is detected the better off you will be.
Having a close family member with AMD may increase your chances of having the disease as much as 50 percent, making timely diagnosis and treatment imperative.
Other eye diseases that run in families include strabismus (crossed eyes), myopia (nearsightedness), hyperopia (farsightedness), and astigmatism.
All of these family connections are important to know so that you and your eye doctor can together take the best possible care of your eyes. Before your next eye exam, ask your relatives if they have a history of eye disease. It might not make for the lightest of conversation at your next family gathering, but it could help save your vision.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Do you have family members with eye-related conditions?
The two main eye diseases in adults that have a genetic link are glaucoma and age-related macular degeneration (AMD).
Glaucoma is a deterioration of the optic nerve caused by pressure in the eye or poor blood flow to the optic nerve. It has no symptoms at its onset. In most cases if you wait to get glaucoma diagnosed until you begin to realize there is something wrong with your vision, upwards of 70% of your optic nerve will have already been destroyed. Once the nerve is destroyed there is no way of reversing that today and treatment is focused on trying to preserve whatever nerve tissue is left.
Your chances of getting glaucoma are four to 10 times higher if you have a close relative with glaucoma. Getting your eyes examined regularly is always important but even more so if there is a family history of glaucoma.
Macular degeneration is the leading cause of blindness in most of the developed world. It too can cause serious vision loss if you wait until you have significant symptoms before a diagnosis. There are now some preventative treatments for AMD--the earlier it is detected the better off you will be.
Having a close family member with AMD may increase your chances of having the disease as much as 50 percent, making timely diagnosis and treatment imperative.
Other eye diseases that run in families include strabismus (crossed eyes), myopia (nearsightedness), hyperopia (farsightedness), and astigmatism.
All of these family connections are important to know so that you and your eye doctor can together take the best possible care of your eyes. Before your next eye exam, ask your relatives if they have a history of eye disease. It might not make for the lightest of conversation at your next family gathering, but it could help save your vision.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Millions of people are affected by dry eye syndrome and the prevalence of dry eye increases with age. An estimated 3.2 million women and over and 1.68 million men age 50 and over are affected by dry eye syndrome.
Here are some risk factors for dry eye:
Aging: Advancing age is the single most important risk factor for dry eye. Most of our body’s moisture-producing glands produce less moisture as we age.
Gender: Women are twice as likely as men to suffer from dry eye. Changes in hormone levels throughout your lifetime often affect the amount of moisture produced by the lacrimal glands that produce tears.
Medical problems: Several diseases result in increased risk for dry eye syndrome, including rheumatoid arthritis, diabetes, thyroid abnormalities, asthma, cataracts, glaucoma, and lupus.
Medication: Certain medications can decrease the body's ability to produce lubricating tears.
Contact lenses: Dry eye is the leading cause of contact lens discomfort or intolerance.
Environmental conditions: Exposure to smoke, fluorescent lights, air pollution, wind, heat, air conditioning, and dry climates can increase tear evaporation.
Computer users: People who spend many hours staring at computer screens tend to blink significantly less often. Not blinking allows the eyes to dry faster.
Refractive surgery: This increases the risk of dry eye. Surgery often interferes with the superficial nerves on the cornea. Properly functioning nerves are necessary to help keep the eye surface moist.
Dry eye can present in many different ways. You can have irritation (often presenting as a foreign body feeling on the eye surface), redness, burning, excessive tearing (yes, that sounds counterintuitive but dry eye often presents this way), or intermittent blurring of vision.
The only way to be sure your symptoms are truly a dry eye problem is to have a comprehensive exam by your ophthalmologist or optometrist. There are other problems, such as allergic reactions and blepharitis, that can create similar symptoms so you need to be examined to determine which of these issues is causing your symptoms.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Ocular allergies are among the most common eye conditions to hit people of all ages.
Though typically worse in the seasons of Spring and Summer, some people suffer with allergies all year. This is especially true for people who have allergies to pet dander, mold, dust mites, and other common allergens that tend to linger throughout the year.
The hallmark sign of ocular allergies is itching.
While itching can be a symptom of other eye conditions, the likelihood that there is at least some allergy component to the condition is quite high. This seems to be particularly true when the itching occurs mainly in the inner corner of the eyes. This signals that the condition is allergy-related, whereas itching along the eyelid margin suggests other conditions.
Allergy itching is usually accompanied by redness, tearing, and string-like mucus discharge from the eye. When accompanied by rhinitis, sinusitis, and sneezing, people can truly suffer from their allergies - especially as it relates to the eye.
The good news is there are numerous avenues for relief from this annoying condition.
There are many over-the-counter antihistamine drops. Talk to your eye doctor about which ones are recommended.
In particularly severe cases, prescription antihistamine/mast cell stabilizer combination drops, or even topical steroids, can be used. In addition, cold compresses can be a great therapy in combination with the drops.
Article contributed by Dr. Jonathan Gerard
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

In light of the holiday season, here are our top 10 eye care jokes.
1) What do you call a blind deer? No Eye Deer!
2) What do you call a blind deer with no legs? Still No Eye Deer!
3) Why do eye doctors live long lives? Because they dilate!
4) Why did the blind man fall into the well? He couldn’t see that well.
5) Why shouldn’t you put avocados on your eyes? Because you might get guac-coma!
6) What did the right eye say to the left eye? "Between you and me, something smells."
7) A man goes to his eye doctor and tells the receptionist he’s seeing spots. The receptionist asks if he’s ever seen a doctor. The man replies, “No, just spots.”
8) How many eye doctors does it take to screw in a light bulb? One … or two
9) Unbeknownst to her, a woman was kicked out of peripheral vision club. She didn’t see that one coming!
10) What do you call a blind dinosaur? A do-you-think-he-saurus
Bonus: What do you call a blind dinosaur’s dog? A do-you-think-he-saurus rex!
Article contributed by Dr. Jonathan Gerard
Shingles is the term we use to describe a condition that is caused by a re-activation of the Herpes Varicella-Zoster virus. The origin of this infection usually goes way back to childhood with a disease we know as chickenpox.
When you have a chickenpox infection your immune system manages to eventually suppress that virus from causing an active infection, but the virus does not get completely eliminated from your body--it is able to go and hide in your nerve roots.
Your immune system manages to keep the virus in check for most of your life but there may come a time in adulthood when your immune system is not working as well as it used to, and the virus can reappear. It usually does this along the distribution of a single sensory nerve called a dermatome.
The most common area for this to occur is along your trunk (chest or abdomen) but it is also commonly found on the face.
There are three branches of nerves that supply sensation to your face. They are all branches of the fifth cranial nerve. Those three branches supply the upper face (V1), the mid face (V2), and the lower face (V3). Most of the time, shingles breaks out along only one of the branches at a time. The one that most frequently involves the eye is a rash breakout in the V1 distribution. This can involve the forehead and both the upper and lower eyelid. It is also much more likely that the inside of the eye will be involved if the tip of the nose has a lesion on it. The reason for that is that there is a specific subbranch of the V1 nerve called the nasocilliary nerve. This nerve is responsible for sensation on the tip of the nose and the inside of the eye.
The hallmark of shingles is that once the rash erupts it stays on one side of the body, including when it happens on the face. The rash will go up to the centerline of your face but will not go to the other side. You may get lesions on your scalp, but they will not show up on the back of your head. That is because the V1 does not go past half way back on your scalp. The back of your head has its sensation handled by nerves that come out of your spinal cord not cranial nerves that come out of the front of your skull.
Many people have a hard-to-describe sensation of pain, irritation, or itching along the distribution of the nerve for a day or two before the rash shows up. It is important to recognize the rash as quickly as possible because the drugs that treat shingles--usually Acyclovir, Famvir (famciclovir), or Valtrex (valacyclovir)--are much more effective if they are started within three days of the beginning of the rash.
Eye problems may occur along with the rash, especially if there is a lesion on the tip of the nose.
The two biggest problems are swelling or inflammation of the cornea and inflammation inside the eye, which we call iritis or uveitis.
The inflammation in the eye can cause pain and it can also increase eye pressure and cause glaucoma. Most often the treatment for the eye problem is to use the same oral medication mentioned above and sometimes it also can require eye drops to decrease the inflammation the virus is causing (steroid drops) or drops to try and lower the elevated pressure (glaucoma drops).
The eye inflammation can cause blurred vision, pain, and significant light sensitivity. It can be hard to treat and control and can continue to be a problem long after the skin lesions are gone. In fact, many times problems don’t even start until the skin lesions are starting to go away.
It is recommended that if you have shingles affecting the distribution of V1, you should have an eye exam within a few days of the diagnosis being made and then another exam again a week later because, as mentioned above, the eye problems can present a week later than the skin eruptions.
There can be some serious long-term effects of shingles on your eye, including glaucoma and corneal scarring that can be bad enough to require a corneal transplant. The symptoms are often obvious with the vision being blurry and the eye being very red and painful, but sometimes the symptoms may be much more mild even when significant trouble is brewing inside the eye. So even if you think the eye feels fine, you need an exam to ensure there is not subtle inflammation or significant elevation of the pressure in the eye.
The other long-term problem with shingles around the eye is the possibility of there being ongoing pain in the area that can last for many years. This is called Post Herpetic Neuralgia (PHN). This pain can occur all along the dermatome where shingles had occurred. The eye itself may look perfectly normal but the pain persists. This is often treated with drugs that were originally developed as seizure medication but have since been shown to help alleviate neurological pain. The two most commonly used drugs for this are Neurontin (Gabapentin) and Lyrica (Pregabalin).
The most important thing you can do to try and make sure this doesn’t happen to you is to be vaccinated for shingles. The original vaccination called Zostavax has been available since 2006 in the U.S. It is a single-injection vaccine and was recommend for everyone over 60. The main issue with this vaccine is that it only reduced the risk of getting shingles by 51% and PHN by 67%. In 2017 a new vaccine was approved in the U.S. called Shingrix. This vaccine is a two-injection vaccine with the second shot given 2 to 6 months after the first. This vaccine is recommended for everyone 50 years or older. The big advantage of this vaccine is that is 85-97% effective in preventing both shingles and PHN in people with normal immune systems. For more information about this vaccine you can go to the CDC website by clicking here.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Your Eyes Are A Precious Gift--Protect Them During The Holidays
“I want an official Red Ryder, carbine action, two-hundred shot range model air rifle!”
“No, you'll shoot your eye out.”
This line from “A Christmas Story” is one of the most memorable Christmas movie quotes ever. Funny in the movie, but the holiday season does present a real eye injury threat.
For those who celebrate Christmas, that risk begins even before the actual day.
Some of the most frequent holiday-related eye injuries come from the Christmas tree itself.
Holiday eye safety begins with the acquisition of the tree. If you are cutting down your own tree, please wear eye protection when doing the cutting--especially if you are going to be using a mechanical saw, such as a chain saw or sawzall. You need to also be careful of your eyes when loading a tree on top of the car. It is easy to get poked in the eye when heaving the tree up over your head.
Once back at home, take care to make sure no one else is standing close to the tree if you had it wrapped and now need to cut the netting off. The tree branches often spring out suddenly once the netting is released.
Other injuries occur in the mounting and decorating phase. Sharp needles, pointy lights, and glass ornaments all pose significant eye injury risk. If you are spraying anything like artificial tree snow on the branches be sure to keep those chemicals out of your eyes.
Having now successfully trimmed the tree without injury, let’s move our holiday eye safety talk to the toys.
We want to spend the holiday happily exchanging gifts in front of a warm fire, drinking some eggnog, and snacking on cookies--not going to the emergency room with an injury.
The Consumer Product Safety Commission reported there were 254,200 toy-related emergency room visits in 2015, with 45% of those being injuries to the head and face--including the eyes.
In general, here are the recommendations from the American Academy of Ophthalmology in choosing eye-safe toys for gifts:
- “Avoid purchasing toys with sharp, protruding or projectile parts."
- “Make sure children have appropriate supervision when playing with potentially hazardous toys or games that could cause an eye injury."
- “Ensure that laser product labels include a statement that the device complies with 21 CFR (the Code of Federal Regulations) Subchapter J."
- “Along with sports equipment, give children the appropriate protective eyewear with polycarbonate lenses. Check with your eye doctor to learn about protective gear recommended for your child's sport."
- “Check labels for age recommendations and be sure to select gifts that are appropriate for a child's age and maturity."
- “Keep toys that are made for older children away from younger children."
- “If your child experiences an eye injury from a toy, seek immediate medical attention.”
More specifically, there is a yearly list of the most dangerous toys of the season put out by the people at W.A.T.C.H. (world against toys causing harm).
Here are types of toys to avoid:
- Guns that shoot ANY type of projectile. This includes toy guns that shoot lightweight, cushy darts.
- Water balloon launchers and water guns. Water balloons fired from a launcher can easily hit the eye with enough force to cause a serious eye injury. Water guns that generate a forceful stream of water can also cause significant injury, especially when shot from close range.
- Aerosol string. If it hits the eye it can cause chemical conjunctivitis, a painful irritation of the eye.
- Toy fishing poles. It is easy to poke the eyes of nearby children.
- Laser pointers and bright flashlights. The laser or other bright lights, if shined in the eyes for a long enough time, can cause permanent retinal damage.
There are plenty of great toys and games out there that pose much lower risk of injury so choose wisely, practice good Christmas eye safety, and have a great holiday season!
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
There is a common misconception that any adverse reaction to a drug is an allergy. That is definitely not the case.
Reporting to your doctors that you have an allergy to a medication when what you really had was a side effect could potentially create a substantial alteration to your medical care in the future. And this could mean a physician might avoid using a drug that could possibly save your life because of the fear of an allergic reaction.
An anaphylactic allergic reaction generally produces a very specific set of symptoms, including difficulty breathing due to constriction of windpipe, swelling of your tongue, and/or a rash and hives that break out over your body. While an allergic reaction can present in other ways, these are the most frequent reactions that occur when you have a true allergy to something.
If that is not the type of reaction you had then it probably isn’t an allergy. If you are uncertain if your reaction to a medication is an allergy or not, testing by an allergist may be able to tell you if your reaction was a true allergy or a side effect.
It is not always just the patient who can misdianose a side effect as an allergy. Sometimes it is the doctor or the dentist who tells the patient, “You must be allergic.” This is a quick and easy explanation but not always the correct one.
In optimal medicine, there are not always a lot of “lifesaving” incidences, but there are several drugs that are the preferred treatment for certain conditions and if you report an allergy to these drugs it may make your doctor use a much less effective drug.
Here are some specific examples of when a false report of an allergy may lead to less effective treatment or even failure to offer life-saving treatment.
Epinephrine
The most common potential “lifesaving” drug to which patients sometimes report an allergy to is Epinephrine.
The story usually goes something like this: “I was having a dental procedure and soon after the dentist injected my mouth with a local anesthetic of lidocaine with epinephrine my heart started racing and pounding out of my chest and I almost passed out.” This hypothetical patient may come to the conclusion or the dentist may mention that the patient is allergic to epinephrine. That reaction is almost never an allergy but a side effect that occurs when a substantial dose of the lidocaine and the epinephrine gets into the blood stream and stimulates the heart.
The mouth and gums are very vascular, and it is easy to have some of that injection end up in the bloodstream, but that reaction is not an allergy and should not be reported as such.
Epinephrine is used to treat severe (anaphylactic) allergic reactions and not using it if you were to ever have a severe allergic reaction could lead to some very bad outcomes. This is not to say you can’t be allergic to epinephrine. You can, but it is extremely rare. If there is any doubt you should be tested by an allergist before you ever record yourself in a medical setting as being “allergic” to epinephrine.
Cortisone/Steroids
Cortisone is a highly effective drug to treat many conditions. Again, it is unlikely but not impossible to be allergic to it.
We all have naturally occurring cortisol circulating in our bodies and cortisone is a very similar molecule but not exactly the same. Cortisone also can have a wide range of side effects depending on where and how it is administered
Some of the common side effects of cortisone, which have been mislabeled as an allergy, are: Making your blood sugar rise, insomnia, mood swings, nausea, and weight gain. These are all known side effects of the drug and not allergies. Cortisone side effects are associated with only certain routes of administration and are often dose dependent.
Why is this important in terms of your eye care? We often use cortisone derivatives, like Prednisolone, to fight inflammation that may occur in your eye, particularly after any ocular surgery. If you report that you are allergic to cortisone when you really only experienced a side effect, we are going to have to use a less-effective medication to deal with your eye inflammation.
As I mentioned above, most side effects are dose dependent and the dose you got in a pill may have caused a side effect you’d rather not have again but the dose in an eye drop is significantly less and highly unlikely to give you the side effect you got with a pill taken orally.
Antibiotics
People often report they are allergic to antibiotics when they really experienced a side effect.
The most common side effect with oral antibiotics is some type of gastrointestinal disturbance, like nausea, or diarrhea. If that was what you had and just prefer not to get that again you still shouldn’t report it as an allergy. If you do, then the drug can’t be used as an eye drop or ointment that might be the best treatment for your condition.
An antibiotic eye drop/ointment is very unlikely to produce the same gastrointestinal trouble that the same antibiotic gave you when given as a pill. You don’t want to take away the most effective treatment for your problem because you mislabeled a side effect as an allergy.
Sedatives/Anesthesia
Most of the time with these drugs the issue is how you felt either during or after a procedure.
Common comments are “it took me too long to wake up” (side effect not an allergy); “the sedative I got in my IV burned when it went in” (side effect not an allergy); “I was sleepy all day” (side effect not an allergy); “I was nauseous after the procedure” (could be an allergy but much more likely to be a side effect).
Why are these important? We can make you much more comfortable for a local anesthesia procedure if we can use some sedation. Using sedation may be better for you and the doctor performing the surgery because you are much less likely to move during the surgery if you are resting comfortably.
If you ever have an untoward reaction to a medication it is worth your time and effort to really probe into the issue to figure out if what you had was really an allergy or just a side effect because sometimes your life may depend on it.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Read more: The Importance of Knowing if it Was a Side Effect or a True Allergy

There are certain eye conditions where an injection into your eye might be recommended.
Injections into the eye, specifically into the vitreous or gel-filled cavity of the eye, are called intravitreal injections.
In Part 1 of "You Want to Do WHAT to My Eye?" we talked mostly about anti-vascular endothelial growth factor (anti-VEGF) injections. Anti-VEGF injections are probably the most commonly injected agents and they are used to treat wet age-related macular degeneration (ARMD), diabetic retinopathy, and retinal vein occlusion.
But there are other injections that may be used as treatment.
Another injected medication used in combination with Anti-VEGF agents to treat wet macular degeneration, diabetic retinopathy and retinal vein occlusion are steroids. Additionally, steroids can be used to treat inflammation, or uveitis, in the eye. There is a steroid implant called Ozurdex, that looks like a white pellet and can last up to 3 months in the eye. The downside of steroids is that they can increase eye pressure and cause progression of cataracts.
Antibiotics are another type of medication that can be injected into the eye. Sometimes an infection called endophthalmitis can develop inside the eye. This can occur after eye surgery or a penetrating injury to the eye. The presenting signs and symptoms of endophthalmitis are loss of vision, eye pain and redness of the eye. Bacteria is usually the cause of the infection, and antibiotics are the treatment. The best way to deliver the antibiotics is to inject them directly into the eye.
Another relatively new injection is Jetrea, an enzyme that breaks down the vitreous adhesions that may develop on the surface of the retina. As we age, the vitreous contracts away from the retinal surface. When this occurs over the macula, the region responsible for fine vision, the result is visual distortion. Jetrea is an injection that will dissolve the vitreous adhesions and relieve the traction on the retina. Prior to the advent of Jetrea, the only treatment would have been surgery to physically remove the vitreous jelly and traction on the retina.
The next time you visit your eye doctor and are told you need an injection of medication, it will likely be one of the above agents.
Article contributed by Dr. Jane Pan

There are some eye conditions where your doctor might recommend an eye injection as a treatment option.
Injections into the eye, specifically into the vitreous or gel-filled cavity of the eye, are called intravitreal injections.
Anti-vascular endothelial growth factors (anti-VEGF) are probably the most commonly injected agents. They are used to treat wet age-related macular degeneration (ARMD), diabetic retinopathy, and retinal vein occlusion.
In these conditions, there are abnormal leaky blood vessels that cause fluid and blood to accumulate in and under the retina. This accumulation of fluid results in loss of central vision. The role of anti-VEGF agents is to shrink these abnormal vessels and restore the normal architecture of the retina.
Three anti-VEGF agents that are widely administered are Lucentis, Avastin, and Eylea.
Lucentis (Ranibizumab) is FDA approved for treatment of wet ARMD, diabetic retinopathy, and vein occlusion. It is specially designed for injection into the eye and is a smaller molecule than Avastin so it may have better penetration into the retina.
Avastin (Bevacizumab) was originally approved by FDA for treating colorectal cancer. It is used “off-label” for the same treatment indications as Lucentis. Off-label usage of medication is legal, but pharmaceutical companies can't promote a medication for off-label use. The amount of Avastin needed for eye injections is a fraction of the amount used to treat colorectal cancer, therefore, the cost of ophthalmic Avastin is only a fraction of the cost of Lucentis. This means that Avastin needs to be prepared sterilely into smaller doses by an outside pharmacy prior to injection into the eye.
Eylea (Aflibercept) is the third anti-VEGF agent. It was designed to have more binding sites than Avastin and Lucentis so it may last longer in the eye than the former two. Eylea is FDA approved for treatment of wet ARMD, diabetic disease, and vein occlusion, and therefore, the cost of Eylea is similar to the cost of Lucentis.
There are also newer agents on the market. Your doctor will deterine which might work best for you.
There is a thought that after prolonged injections, some patients may develop resistance to one particular agent but still respond to the a different agent. Therefore, your ophthalmologist will individualize your treatment.
Article contributed by Dr. Jane Pan
One of the most commonly asked questions in an eye exam comes right after the refraction, or glasses prescription check: “What is my vision?”
Almost invariably, people know the term “20/20”. In fact, it’s a measure of pride for many people. “My doctor says I have 20/20 vision.” Or, on the other side of that same coin, having vision that is less than 20/20, say 20/400, can be a cause of great concern and anxiety. In this discussion I will describe what these terms actually mean.
To lay the foundation, let’s discuss some common terms. Visual acuity (VA) is clarity or sharpness of vision. Vision can be measured both corrected (with glasses or contact lenses) and uncorrected (without glasses or contact lenses) during the course of an eye exam. The result of an eye exam boils down to two different but related sets of numbers: your VA and your actual glasses prescription.
The notation that doctors use to measure VA is based off of a 20-foot distance. This is where the first 20 in 20/20 comes from. In Europe, since they use the metric system, it is based on meters. The 20/20 equivalent is 6/6 because they use a 6-meter test distance. The second number is the smallest line of letters that a patient can read. In other words, 20/20 vision means that at a 20-foot test distance, the person can read the 20/20 line of letters.
The technical definition of 20/20 is full of scientific jargon - concepts such as minutes of arc, subtended angles, and optotype size. If you’d like to read more of the technical details there is a well-written article with illustrations by Dr. John Ellman, you can find here. For the purposes of our discussion here I’ll try to explain it in less technical terms.
“Normal” vision is somewhat arbitrarily set as 20/20 (some people can see better than that). Let’s say you have two people: Person A with 20/20 vision and Person B with 20/40 vision. The smallest line of letters that person B can see at 20 feet is the 20/40 line. Person A, with “normal” 20/20 vision, could stand 40 feet away from that same line and see it. There is somewhat of a linear relationship in that the 20/40 letters are twice the size of the 20/20 letters and someone with normal vision could see a 20/40 letter at twice the distance as the person with 20/40 vision.
So how does this translate to a glasses prescription?
Eye doctors can often estimate what your uncorrected VA will be based on your glasses prescription. This works mainly for near-sightedness. Essentially, every quarter step of increasing glasses prescription (i.e. -1.25 as compared to -1.50) means a person can see one less line on a VA chart.
A prescription of - 1.25 works out to roughly 20/50 vision, -1.50 to 20/60 and so on. Anybody with an anatomically sound eyeball, meaning the absence of any kind of disease process, should generally be correctable to 20/20 with glasses or contact lenses. It is important to note, however, that rarely a person’s best corrected VA may be less than 20/20 with no noticeable signs of disease.
Far-sightedness is more difficult to estimate because it is affected by a number of other factors, including one’s age and focusing ability. But that’s a topic for another article.
So there you have it! Hopefully this has shed some light on what these measurements that we take actually mean, and it has allowed you to understand your eye health a little bit better.
Article contributed by Dr. Jonathan Gerard

