
There is an old adage in the eye care industry--Glasses are a necessity, contact lenses are a luxury. Ninety-nine percent of the time this is absolutely true. In the absence of unusual eye disorders or very high prescriptions that don’t allow a person to wear glasses comfortably, contact lenses should only ever be worn if there is a good, sturdy, updated set of prescription glasses available, too. This is due to the fact that there are often emergencies where people cannot wear their contact lenses.
In the 21st century, contact lens technology has gotten to the point where we have drastically cut down on the number of adverse events related to contact lens wear. However, human beings were not meant to wear little pieces of plastic in their eyes. Contact lenses are still considered a foreign body in the eye, and sometimes with foreign bodies, our eyes might feel the need to fight back against the “invader.” As such, issues like red eyes, corneal ulcers, eyelid inflammation, dry eyes, and abnormal blood vessel growth can result from wearing contact lenses.
More often than I would like, I have patients who are longtime contact lens wearers come in, and when I inquire as to the condition of their glasses, they say they don’t own any. My next question is inevitably, “What happens if you get an eye infection and you can’t wear your contacts?” I then see the proverbial light bulb go off in their heads followed by a blank stare. Why? “Because I’ve never had a problem before.” Well, just because you maybe have never been in a car accident before, doesn’t mean you shouldn’t wear your seat belt!
I will therefore repeat the most important takeaway here--Glasses are a necessity, contacts are a luxury. Even if you don’t want to go “all out” and get the most expensive frames or lenses in your glasses, having a reliable pair of glasses is an absolute must for any contact lens wearer.
Article contributed by Dr. Jonathan Gerard
In light of the holiday season, here are our top 10 eye care jokes.
1) What do you call a blind deer? No Eye Deer!
2) What do you call a blind deer with no legs? Still No Eye Deer!
3) Why do eye doctors live long lives? Because they dilate!
4) Why did the blind man fall into the well? He couldn’t see that well.
5) Why shouldn’t you put avocados on your eyes? Because you might get guac-coma!
6) What did the right eye say to the left eye? "Between you and me, something smells."
7) A man goes to his eye doctor and tells the receptionist he’s seeing spots. The receptionist asks if he’s ever seen a doctor. The man replies, “No, just spots.”
8) How many eye doctors does it take to screw in a light bulb? One … or two
9) Unbeknownst to her, a woman was kicked out of peripheral vision club. She didn’t see that one coming!
10) What do you call a blind dinosaur? A do-you-think-he-saurus
Bonus: What do you call a blind dinosaur’s dog? A do-you-think-he-saurus rex!
Article contributed by Dr. Jonathan Gerard
Red, Itchy, swollen eyelids are often due to a condition called blepharitis. Blepharitis tends to be a chronic condition due to thick eyelid mucous gland production that sticks to the bases of the eyelashes. This adherent mucous can allow bacteria to overgrow and also attract and retain allergens. The standard treatment for blepharitis is doing warm compresses and cleaning off the eyelids with a mild baby shampoo and water solution. This treatment works for some people but there are many more sufferers who have chronic irritation and relapses despite this treatment. If the warm compresses and eyelid scrubs are not quite keeping the condition under control there are several other additional treatments that can be used to control the symptoms. One such treatment that your doctor may decide upon is to use an antibiotic/steroid combination drop or ointment. We usually use these for short periods of time to try to bring the condition under control. They are not good to use chronically because it can build resistant bacteria and the steroid component can cause other eye issues like cataracts and glaucoma. The treatment is very safe for short term use but chronic use is usually not a good option. There are also antibiotic eyelid scrubs such as Avenova which can be prescribed and used on a more long-term basis. Oral Doxycycline can also be used longer in very low doses. Doxycycline is an antibiotic that when used to treat infections is generally prescribed in a dose of 100mg twice a day. For chronic Blepharitis suffers we generally use a much lower dose of around 50 mg a day. At that dose we are using the Doxycycline to help thin out the mucous production from the eyelid glands more than for its antibiotic properties. In summary, blepharitis can be a chronic issue that requires some persistent “maintenance” work be done to keep it under control, with further intervention sometimes needed for flare-ups.
Article contributed by Dr. Brian Wnorowski, M.D.
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ
Choroidal nevus is the fancy term for a freckle in the back of the eye.
This lesion arises from a collection of cells that make pigment in the choroid, which lines the back of the retina and supplies the retina with nutrients. These choroidal nevi (plural of nevus) are usually grayish in color and develop in about 5-10% of the adult population. They are usually asymptomatic and detected during a routine dilated eye exam.
Just like any freckle on our body, we should monitor it for any change in size or growth. This is usually done with a photograph of the nevus and annual exams are normally recommended to monitor any change.
In addition to a photograph, other tests that can be used to monitor the nevus are:
- Optical coherence tomography - a test that uses light waves to take cross-section pictures of the retina. This test is used to detect if the nevus is elevated or if fluid is present underneath the retina.
- Ultrasound - uses sound waves to measure the size and elevation of the nevus.
- Fluorescein angiography - a dye test to detect abnormal blood flow through the nevus.
The concern is for transformation of the choroidal nevus into melanoma, a cancer in the eye. It has been estimated that 6% of the population have choroidal nevus and 1 in 8,000 of these nevi transform into melanoma. Some factors predictive of possible transformation in melanoma are:
- Thickness of the lesion, greater than 2 mm.
- Subretinal fluid, observed on exam or optical coherence test.
- Symptoms that include decreased or blurry vision, flashes, or floaters.
- Orange pigment in the lesion.
- Located near the optic nerve.
Early detection of choroidal melanoma results in earlier treatment and better outcomes for the patient. Many times, a patient with choroidal melanoma may be asymptomatic, and so routine dilated eye exams should be performed to identify any suspicious choroidal nevus.
In general, there is no treatment for choroidal nevus other than observation and monitoring for change. Therefore, a visit to your eye doctor is recommended to detect any freckles in the back of your eye.
Article contributed by Dr. Jane Pan

A common in-office procedure is an eye injection for treatment of various eye conditions, such as wet macular degeneration, diabetic retinopathy, or vein occlusion.
It is normal to be anxious prior to your first eye injection but knowing what to expect may alleviate some anxiety.
Your eye will be numbed with topical anesthetic drops. Usually, a cotton-tipped applicator soaked in anesthetic will be held against the white part of the eye to numb it. Sometimes, a thick gel may also be used for numbing. Once the eye is numbed, it will then be cleaned and a small instrument will be used to hold the eye open. During the actual injection, some patients feel pressure while others may feel a quick sting. Each person will have a different experience and each injection will be different.
The medicine is injected into the white part of the eye. Sometimes a blood vessel may be encountered during the injection and you may notice a little redness on the outside of the eye. This is purely a cosmetic symptom and the redness will disappear within the next couple of days. Patients may also experience some mild irritation after the injection due to the drops that are placed in the eye. I usually recommend over-the-counter artificial tears to use after the injections. Usually, the eye should feel normal by the next day.
Another common symptom after an injection are floaters. These floaters usually appear as small bubbles in the lower half of your vision, but they will disappear in in a day or two.
There are no activity restrictions after the injection and no antibiotic drops are needed.
Things to watch for after the injection:
- If your eye gets painful or redness develops a couple of days after the injection, then you should call your doctor.
- If your vision declines or you notice increased or hundreds of floaters then you should call to be seen.
Otherwise, patients are usually initially seen once a month after they first start injections
Article contributed by Dr. Jane Pan
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

A common question asked during the eye exam is, “When is the puff coming?”
Patients are referring to air-puff or non-contact tonometry. Tonometry is the procedure used to measure eye pressure, and this is important for diagnosing and monitoring glaucoma.
In non-contact tonometry, a puff of air is used to measure the pressure inside the eye. The benefit of this test is there is no actual contact with the eye, but the air puff is sometimes very startling for patients. Most people hate that test and it isn’t the most accurate way to measure your eye pressure.
Some doctors don’t even use the air-puff test. Instead, they place a yellow drop that consists of a numbing medicine and then shine a blue light on the eye. This is done in front of the slit lamp and a small tip gently touches the eye to measure the eye pressure. This procedure is called Goldmann tonometry and is considered the gold standard for measuring eye pressure.
Another method for checking eye pressure is the Tonopen. This is a portable, hand-held instrument that is useful when patients can’t sit in front of the slit lamp to have their eye pressure checked. The Tonopen also requires a numbing drop to be placed in the eye, and the tip gently touches the eye.
A common question related to tonometry is “what normal eye pressure?”
Normal eye pressure ranges from 10-21 mm Hg. Eye pressure doesn't have any relationship to blood pressure. Many times, people are surprised that their eye pressure is high, but they have normal blood pressure. In general, there is no diet or exercise that will significantly affect eye pressure. It is therefore important to have your eye pressure checked regularly because there are usually no symptoms of high eye pressure until it has affected your vision.
Article contributed by Dr. Jane Pan
Read more: Why Do You Have to Touch My Eye or Puff It with Air?
Not everyone understands the importance of sunglasses when the weather turns cold.
Polarized sunglasses are usually associated with Summer, but in some ways it is even more important to wear protective glasses during the Winter.
It’s getting to be that time of year when the sun sits at a much different angle, and its rays impact our eyes and skin at a lower position. This translates to an increase in the exposure of harmful UV rays, especially if we are not wearing the proper sunglasses as protection.
Polarized sunglasses, which are much different than the older dye-tinted lenses, are both anti-reflective and UV resistant. A good-quality polarized sunglass lens will protect you from the entire UV spectrum. This not only preserves your vision, but it also protects the skin around the eyes, which is thought to have a much higher rate of susceptibility to skin cancer.
Snow poses another issue that can be countered by polarized sunglasses.
Snow on the ground tends to act as a mirror because of its white reflective surface and this reflection can become a hindrance while driving. The anti-reflective surface of polarized sunglasses helps reduce the glare and gives drivers improved visibility.
Polarized sunglasses come in many different options based on a patient’s needs. Whether it’s single-vision distance lenses, bifocals, or progressive lenses, there is a polarized lens for every patient.
Winter is a great time of year to ask your optical department about purchasing polarized sunglasses.
Article contributed by Richard Striffolino Jr.
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ
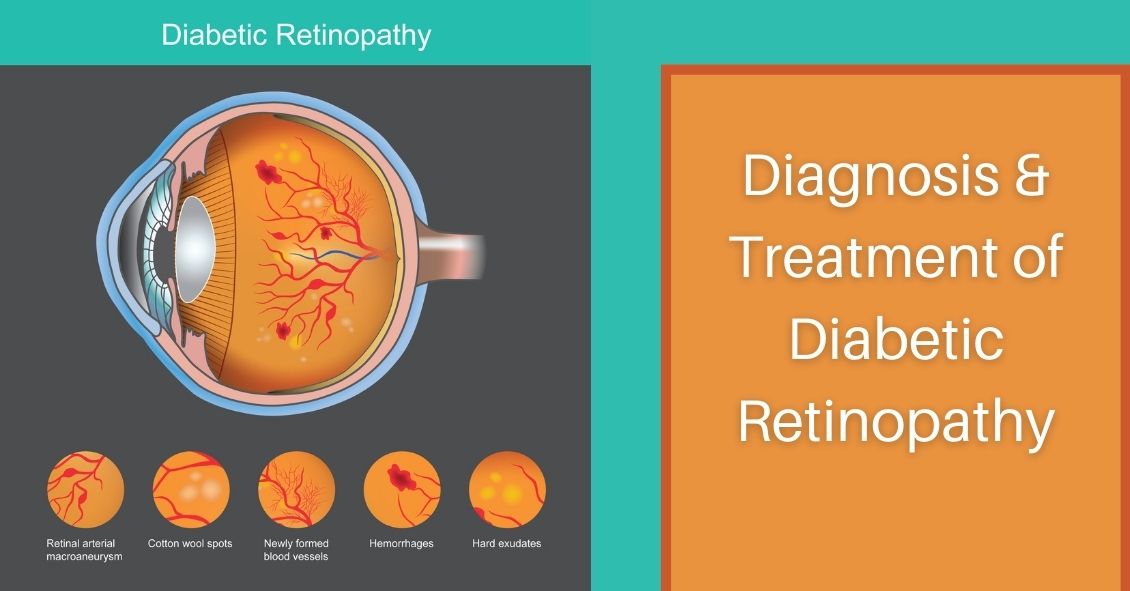
Diabetic retinopathy, which is a complication of diabetes that affects the eyes, is detected during a comprehensive eye exam that includes:
- Visual acuity testing.
- Dilated exam in which drops are placed to widen the pupil to allow examination of the retina.
- Tonometry. Measurement of the eye pressure inside the eye.
Supplemental testing may include:
- Optical coherence tomography (OCT). This is a non-invasive test that images the retina to detect any fluid or diabetic macular edema.
- Fluorescein Angiography. This test involves an injection of a dye into your arm and a series of pictures that are taken as the dye flows through the retinal vessels. This may show leakage of fluid or the growth of new blood vessels in the retina.
Treatment for Diabetic Retinopathy
The best treatment is prevention of diabetic retinopathy by strict control of blood sugars. Once diabetic retinopathy is present, treatment of diabetic retinopathy will slow progression but won’t cure it.
Diabetic macular edema can be treated with several different therapies that may be used alone or in combination.
These include:
- Injection therapy. Anti-VEGF drugs are injected into the eye to block a substance called vascular endothelial growth factor (VEGF). This medication will block abnormal blood vessel growth and decrease the leakage of fluid into the retina. The three most commonly used drugs include Avastin, Lucentis and Eylea. Steroids are another option for treatment of diabetic macular edema but are used less often due to side effects of possible cataracts and increased eye pressure.
- Laser therapy. Small laser burns are applied in the area of the retinal swelling to slow the leakage of fluid. Laser treatment can be combined with anti-VEGF injections.
Proliferative diabetic retinopathy can be treated with:
- Laser therapy. Laser is applied on the retina to shrink the new blood vessels and to prevent bleeding inside the eye. Bleeding inside the eye will cloud the vision and cause floaters, which are small moving spots that appear in your field of vision.
- Surgery. When there is significant amount of blood or scar tissue inside the eye, then a vitrectomy surgery is performed to remove the blood and scar tissue. Laser and anti-VEGF therapy may also be applied during the surgery.
In the end, the best treatment is prevention of diabetic retinopathy. An annual comprehensive dilated eye exam is recommended for anyone who has been diagnosed with diabetes, since early mild non-proliferative diabetic retinopathy can show no symptoms.
Article contributed by Jane Pan M.D.
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ
Parkinson’s disease is a progressive degenerative condition of the neurological system. The majority of Parkinson’s effects are on movement, often starting off very slowly and subtly. One of the earliest symptoms is a slight tremor in one or both hands. Other early symptoms include a lack of facial expression and decreased blinking of the eyes, so it looks like the person is always staring.
The next stage usually results in difficulty with initiating movement, especially walking. It frequently looks like it takes a tremendous concentrated effort to initiate walking and the steps often start off very small with a shuffling of the feet. At the same time, the disease stiffens the muscles of the arms so that when the person is walking there is a noticeable decrease in the swinging of the arms. Speech becomes much softer and writing becomes more of an effort, with handwriting getting smaller and smaller as the disease progresses.
Parkinson’s can also affect your visual performance, mainly in two parts of your eyes: the tear film and the ocular muscles.
It affects your tear film because of the decreased rate of blinking. The tear film is an important component of your optical system. It coats the surface of the cornea and if it is not smooth and uniform the result is a blurring of your vision. Blinking helps refresh your tear film and spreads it out uniformly. It is analogous to the washers and wipers on your car. If the windshield (like your cornea) is spotty you have a hard time seeing through that windshield. Turn on the washers and now there is more moisture on the surface but that is also spotty and hard to see through until the wipers go by and spread the moisture out evenly. That is very similar to how your cornea, tear film and your eyelids blinking interact to keep your vision clear.
If you don’t blink enough, the tear film begins to dry out in spots and having dry spots next to moist spots results in an irregular film and therefore blurred vision. That is how the decreased blinking frequency in people with Parkinson’s disease results in a complaint of intermittent blurred vision.
The other way the disease affects your vision is by creating a problem called convergence insufficiency. When you read, your two eyes turn inward toward each other in a process called convergence. Your eye muscles are activated in order to have the two eyes point inward to focus on the near object. By interfering with the interaction between your nerves and muscles, Parkinson’s makes it difficult to both initiate and sustain the convergence you need to keep both eyes focused on a near object.
This sometimes results in a disconnect between what a person is capable of reading on an eye chart for a short period of time and what happens after trying to sustain the effort over a longer period of time. This disconnect can result in some frustration. Often during an exam, a quick look at the distance eye chart allows the patient to see fairly well because the dry eye may not be causing any blurring if the patient just blinked a few times before reading the chart. A patient may also do well on the near chart because they are often being tested one eye at a time. When you read things up close with just one eye there is no need for the eyes to converge so they do well one eye at a time.
There are some other less-frequent eye problems that can occur with Parkinson’s. One is called blepharospasm, where the eyelids on either one side or both forcefully close involuntarily. A person can also end up with a condition called apraxia of eye opening, where they can’t voluntarily open the eyelids. This is different from blepharospasm because in this condition the lids are not being forcefully closed, they just won’t open when you want them to.
The majority of these problems do improve if the Parkinson’s is treated with medication or even brain stimulation.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided on this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Shingles is the term we use to describe a condition that is caused by a re-activation of the Herpes Varicella-Zoster virus. The origin of this infection usually goes way back to childhood with a disease we know as chickenpox.
When you have a chickenpox infection your immune system manages to eventually suppress that virus from causing an active infection, but the virus does not get completely eliminated from your body--it is able to go and hide in your nerve roots.
Your immune system manages to keep the virus in check for most of your life but there may come a time in adulthood when your immune system is not working as well as it used to, and the virus can reappear. It usually does this along the distribution of a single sensory nerve called a dermatome.
The most common area for this to occur is along your trunk (chest or abdomen) but it is also commonly found on the face.
There are three branches of nerves that supply sensation to your face. They are all branches of the fifth cranial nerve. Those three branches supply the upper face (V1), the mid face (V2), and the lower face (V3). Most of the time, shingles breaks out along only one of the branches at a time. The one that most frequently involves the eye is a rash breakout in the V1 distribution. This can involve the forehead and both the upper and lower eyelid. It is also much more likely that the inside of the eye will be involved if the tip of the nose has a lesion on it. The reason for that is that there is a specific subbranch of the V1 nerve called the nasocilliary nerve. This nerve is responsible for sensation on the tip of the nose and the inside of the eye.
The hallmark of shingles is that once the rash erupts it stays on one side of the body, including when it happens on the face. The rash will go up to the centerline of your face but will not go to the other side. You may get lesions on your scalp, but they will not show up on the back of your head. That is because the V1 does not go past half way back on your scalp. The back of your head has its sensation handled by nerves that come out of your spinal cord not cranial nerves that come out of the front of your skull.
Many people have a hard-to-describe sensation of pain, irritation, or itching along the distribution of the nerve for a day or two before the rash shows up. It is important to recognize the rash as quickly as possible because the drugs that treat shingles--usually Acyclovir, Famvir (famciclovir), or Valtrex (valacyclovir)--are much more effective if they are started within three days of the beginning of the rash.
Eye problems may occur along with the rash, especially if there is a lesion on the tip of the nose.
The two biggest problems are swelling or inflammation of the cornea and inflammation inside the eye, which we call iritis or uveitis.
The inflammation in the eye can cause pain and it can also increase eye pressure and cause glaucoma. Most often the treatment for the eye problem is to use the same oral medication mentioned above and sometimes it also can require eye drops to decrease the inflammation the virus is causing (steroid drops) or drops to try and lower the elevated pressure (glaucoma drops).
The eye inflammation can cause blurred vision, pain, and significant light sensitivity. It can be hard to treat and control and can continue to be a problem long after the skin lesions are gone. In fact, many times problems don’t even start until the skin lesions are starting to go away.
It is recommended that if you have shingles affecting the distribution of V1 that you have an eye exam within a few days of the diagnosis being made and then again a week later because, as mentioned above, the eye problems can present a week later than the skin eruptions.
There can be some serious long-term effects of shingles on your eye, including glaucoma and corneal scarring that can be bad enough to require a corneal transplant. The symptoms are often obvious with the vision being blurry and the eye being very red and painful, but sometimes the symptoms may be much more mild even when significant trouble is brewing inside the eye. So even if you think the eye feels fine, you need an exam to ensure there is not subtle inflammation or significant elevation of the pressure in the eye.
The other long-term problem with shingles around the eye is the possibility of there being ongoing pain in the area that can last for many years. This is called Post Herpetic Neuralgia (PHN). This pain can occur all along the dermatome where shingles had occurred. The eye itself may look perfectly normal but the pain persists. This is often treated with drugs that were originally developed as seizure medication but have since been shown to help alleviate neurological pain. The two most commonly used drugs for this are Neurontin (Gabapentin) and Lyrica (Pregabalin).
The most important thing you can do to try and make sure this doesn’t happen to you is to be vaccinated for shingles. The original vaccination called Zostavax has been available since 2006 in the U.S. It is a single-injection vaccine and was recommend for everyone over 60. The main issue with this vaccine is that it only reduced the risk of getting shingles by 51% and PHN by 67%. In 2017 a new vaccine was approved in the U.S. called Shingrix. This vaccine is a two-injection vaccine with the second shot given 2 to 6 months after the first. This vaccine is recommended for everyone 50 years or older. The big advantage of this vaccine is that is 85-97% effective in preventing both shingles and PHN. For more information about this vaccine you can go to the CDC website by clicking here.
Article contributed by Dr. Brian Wnorowski, M.D.
Getting your eyes dilated can be inconvenient – dilation makes the eyes light sensitive which can make it difficult to read books or use phones and computers for a couple of hours.
So wouldn’t it be great to have another drop to reverse the effects of dilation?
On Dec. 31, 1990, dapiprazole, under the trade name Rev-Eyes, was approved by the FDA and thought to be the answer to all the post-dilation problems. It was marketed for treatment of medically-induced dilation by stimulating pupillary constriction and restoration of accommodative function for reading.
In clinical practice, dapiprazole took between one to two hours to return pupils to pre-dilation size.
Side effects such as stinging upon instillation, conjunctival hyperemia (redness of eye), headache, and a few instances of ptosis (lid drooping), with a possible additional dollar cost to patients, seemed to lessen dapiprazole’s overall clinical benefit.
Reading ability returned in approximately 43 minutes with dapiprazole vs 66 minutes without the drop (Optom Vis Sci 1994 May; 71(5):319-22). The main complaint that people had after using dapiprazole was the conjunctival hyperemia, which lasted more than three hours. The other issue was that dapiprazole was costly, so some practitioners included an additional charge for the reversal of dilation to offset the cost.
The full adverse reaction profile according to Drugs.com is as follows:
"Adverse Reactions: In controlled studies, the most frequent reaction to dapiprazole was conjunctival injection lasting 20 minutes in over 80% of patients. Burning on instillation of dapiprazole hydrochloride ophthalmic solution was reported in approximately half of all patients. Reactions occurring in 10% to 40% of patients included ptosis, lid erythema, lid edema, chemosis, itching, punctate keratitis, corneal edema, browache, photophobia and headaches. Other reactions reported less frequently included dryness of eyes, tearing and blurring of vision."
Currently, Rev-Eyes is off the market. The FDA has stated that Rev-Eyes was not withdrawn from the market for reasons of safety or effectiveness.
At this time, there is nothing available for reversal of dilation. People who get dilated will still need to wear their sunglasses and to put off reading for a couple of hours until the effects of the dilation drops wear off.
Article contributed by Dr. Jane Pan
This blog provides general information and discussion about eye health and related subjects. The words and other content provided on this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
The tears that coat the surface of your eyes have both a liquid and a mucous layer to them. It is normal to have a small amount of mucus in your tear film. But that mucus can significantly increase when the eye gets irritated.
Some of the most common causes of irritation that can make the eye overproduce mucus are:
- Conjunctivitis, which could be caused by an allergy, bacteria, or virus
- Blepharitis, which is an inflammation of the eyelids
- Dry Eye Syndrome
When any of these conditions occur, the eye will begin to make more mucus.
Sometimes the mucous production really is excessive and there is a temptation to keep pulling it out with either your fingers or a cotton swab. DON'T DO THIS--it will just lead to recurring irritation and problems.
Any mucus that gets deposited OUTSIDE the eye on the outer eyelid or on the lashes is fair game for removal. In fact, anything on the exterior of the eyelid or stuck to the eyelashes should be cleaned off. Just don’t reach INSIDE the eyelids.
Every time you go inside the eye to remove mucus, your finger or a cotton swab further irritates the eye and causes it to make even more mucus and you end up with the viscious cycle that we call mucus fishing syndrome.
If you have an acute problem that is causing excessive mucus, you need to try and get the underlying problems treated and under control. That means treating the allergy, blepharitis, infectious conjunctivitis, or dry eye syndrome.
In addition, you need to STOP putting your fingers in your eye and pulling the mucus out. Sit on your hands if you have to--but you have to stop or it is never going to get better.
If you have gone through treatment for the original problem but still find yourself pulling mucus out of your eye, you may need your doctor to try a steroid drop in order to decrease the production and try to help you get out of the habit of putting your fingers in your eyes.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Fall brings a lot of fun, with Halloween bringing loads of it.
But did you know that some Halloween practices could harm your vision? Take Halloween contacts, for instance. They vary widely, with everything from monster eyes to goblin eyes to cat eyes to sci-fi or a glamour look. They can be just the added touch you need for that perfect costume. However, some people do not realize that the FDA classifies contact lenses as a medical device that can alter cells of the eye and that damage can occur if they are not fit properly.
Infection, redness, corneal ulcers, hypoxia (lack of oxygen to the eye) and permanent blindness can occur if the proper fit is not ensured. The ICE, FTC, and FDA are concerned about costume contacts from the illegal black market because they are often unsafe and unsanitary. Proper safety regulations are strictly adhered to by conventional contact lens companies to ensure that the contact lenses are sterile and packaged properly and accurately.
Health concerns arise whenever unregulated black-market contacts come into the US market and are sold at flea markets, thrift shops, beauty shops, malls, and convenience stores. These contacts are sold without a prescriber's prescription, and are illegal in the US. There have also been reports of damage to eyes because Halloween spook houses sometimes ask employees to share the same pair of Halloween contact lenses as they dress up for their roles.
So the take home message is, have a great time at Halloween, and enjoy the flare that decorative contacts can bring to your costume, but get them from a reputable venue and be fit by an eye care professional with a proper legal prescription. Don't gamble with your eyes for a night of Halloween fun!
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ
Read more: Why Those Cheap Halloween Costume Lenses Aren't Worth the Cost
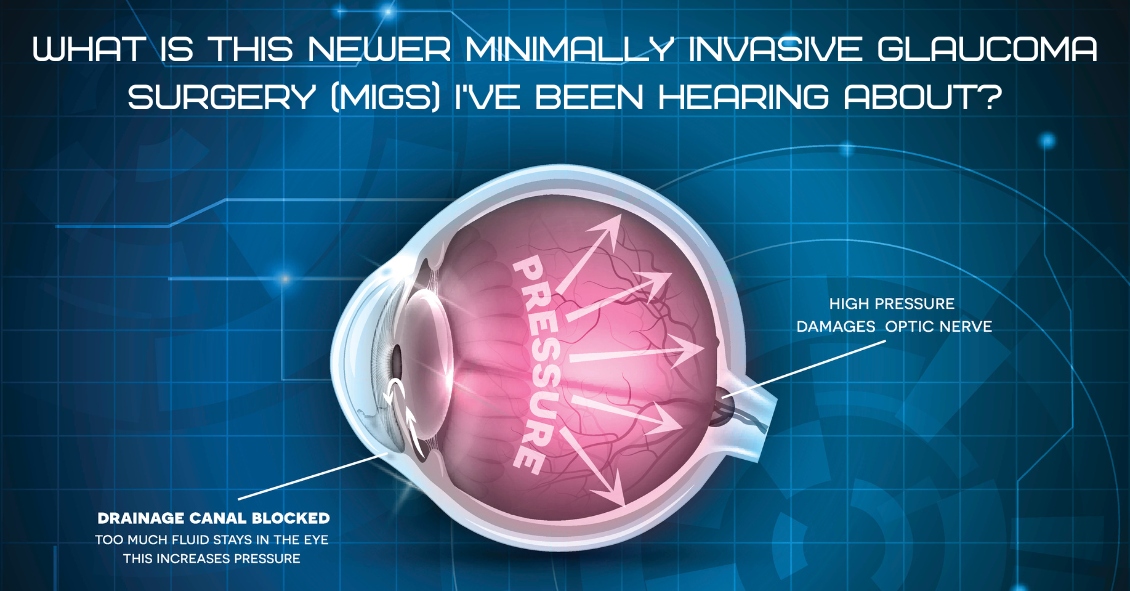
For over 40 years the standard surgical treatment for glaucoma was a procedure called a trabeculectomy.
In a trabeculectomy, the ophthalmic surgeon would make a hole in the wall of eye to allow fluid from the inside of the eye to flow out of the eye and then get resorbed by the blood vessels in the conjunctiva (the mucous membrane that covers the white part of the eye).
This surgery often resulted in a large decrease in the Intraocular Pressure (IOP). Reducing the IOP is the goal of glaucoma surgery because multiple studies show that if you can reduce the pressure the progression of glaucoma slows.
The problem with trabeculectomy is that although it frequently lowers the pressure, it also has a fairly high complication and/or failure rate. This led to some reluctance to perform the procedure unless the glaucoma was severe, or the pressure was very high. As a result of those issues there has been a search during the last 40 years for something that had a lower complication rate and could be more easily deployed earlier in the disease process.
Enter Minimally Invasive Glaucoma Surgery, or MIGS. There are now several types of surgeries that fit in the MIGS category and many of them are used in conjunction with cataract surgery. They are utilized much earlier in the disease process and when combined with cataract surgery they can be used to not only help control the pressure over the long term but can often even reduce the burden of eye drops afterward.
The biggest advantage to MIGS over the trabeculectomy is that when used in conjunction with cataract surgery, MIGS can lower the eye pressure (although not as much as the trabeculectomy) but often with no higher rate of complications as there is with cataract surgery alone.
The lower complication rate is mainly because the MIGS procedures do not create a full-thickness hole in the wall of the eye. Most of them involve putting in some form of stent inside the eye. The stent lets the intraocular fluid get out of the eye more efficiently through its normal internal drain called the trabecular meshwork, rather than having to flow to the outside of the eye as with a trabeculectomy. There are currently several FDA-approved drainage stents with more on the horizon.
A stent is not the only way to lower the pressure along with cataract surgery. There is also a laser treatment you can do from the inside of the eye that slows the amount of fluid the eye makes, which also results in a lower pressure. It is called Endocyclophotocoagulation (ECP). Think of a partially clogged drain in a sink with constantly running water. If you don’t want the sink to overflow (or the pressure in the eye to get too high) you either try to unclog the drain (stent) or you turn down the faucet (ECP).
MIGS has been a great development over the last several years, enabling the ophthalmic surgeon to intervene surgically at a much earlier stage of glaucoma and with a significantly lower complication rate than the more invasive trabeculectomy.
At this point I utilize one of the MIGS procedures in almost all patients who need their cataracts removed and are on one or more glaucoma medications. Even if the glaucoma is fairly well controlled at the time, the MIGS procedure gives us the opportunity to try and get a glaucoma patient off their eye drops, which is both a decreased burden of treatment and lets us keep the eye drops in reserve should the pressure start to increase again later in life.
If you have glaucoma and a cataract you should definitely discuss this with your doctor to see if a MIGS procedure along with your cataract surgery could be the right choice for you.
Article contributed by Dr. Brian Wnorowski, M.D.
Itching, burning, watering, red, irritated, tired eyes... what is a person to do? The symptoms aforementioned are classic sign of Dry Eye Syndrome (DES), which affects millions of adults and children. With increased screen time in all age groups, the symptoms are rising.
What causes this? One reason is that when we stare at a computer screen or phone, our blink reflex slows way down. A normal eye blinks 17,000 times per day. When our eye functions normally, the body usually produces enough tears to be symptom free, however, if you live in a geographical area that is dry, or has a high allergy rate, your symptoms could be worse.
Dry eye syndrome can be brought on by many factors: aging, geographical location, lid hygiene, contact lens wear, medications, and dehydration. The lacrimal gland in the eye that produces tears, in a person over forty years old, starts slowly losing function. Females with hormonal changes have a higher incidence of DES (dry eye syndrome). Dry, arid climates or areas with high allergy causes lend to higher incidences of DES as well.
Blepharities, a condition of the eyelids, can cause a dandruff-like situation for the eye, exacerbating a dry eye condition. Contact lenses can add to DES, so make sure you are in high oxygen contact lens material if you suffer from DES. Certain medications such as antihistamines, cholesterol and blood pressure meds, hormonal and birth control medications, can also cause symptoms of a dry eye. Check with your pharmacist if you are not sure.
And finally, overall dehydration can cause DES. Some studies show we need 1/2 our body weight in ounces of water per day. For example, if you weigh 150 lbs, you need approximately 75 ounces of water per day to be fully hydrated. If you are not at that level, it could affect your eyes.
Treatment for DES is varied, but the main treatment is a tear supplement to replace the evaporated tears. These come in the form of topical ophthalmic artificial tears. Oral agents that can help are Omega 3 supplements such as fish oil or flax seed oil pills. They supplement the function of meibomian glands located at the lid margin. Ophthalmic gels used at night, as well as humidifiers, can help keep your eyes moisturized. Simply blinking hard more often can cause the lacrimal gland to produce more tears automatically.
For stubborn dry eyes, retaining tears on the eye can be aided by punctal plugs. They act like a stopper for a sink, and they are painless and can be inserted by your eye care practitioner in the office. Moisture chamber goggles can also be used in severe cases to hydrate the eyes with their body’s own natural humidity. This may sound far out but it gets the job done.
Being aware of the symptoms and treatments for dry eye syndrome can prevent frustration and allow your eyes to work more smoothly and efficiently in your daily routine. If your eyes feel dry as the Sahara or they water too much, know that help is on the way through proven techniques and products. You do not need to suffer needlessly in the case of Dry Eye Syndrome anymore. Make an appointment to talk with your eye doctor about the best treatments for you!
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

A wrinkle on the retina -- which is also known as an epiretinal membrane (ERM) or a macular pucker -- is a thin, translucent tissue that develops on the surface of the retina.
The retina is the inner layer that lines the inside of the back of the eye and is responsible for converting the light image into an electrical impulse that is then transmitted to the brain. An epiretinal membrane that forms on the retina goes unnoticed by the patient many times, and is only noticed during a dilated eye exam by an eye doctor.
Epiretinal membranes can become problematic if they are overlying the macula, which is the part of the retina that is used for sharp central vision. When they become problematic they can cause distortion of your vision, causing objects that are normally straight to look wavy or crooked.
Causes of a wrinkle on the retina
The most common cause is age-related due to a posterior vitreous detachment, which is the separation of the vitreous gel from the retina. The vitreous gel is what gives the eye its shape, and it occupies the space between the lens and the retina. When the vitreous gel separates from the retina, this can release cells onto the retina's surface, which can grow and form a membrane on the macula, leading to an epiretinal membrane.
ERMs can also be associated with prior retinal tears or detachments, prior eye trauma, or eye inflammation. These processes can also release cells onto the retina, causing a membrane to form.
Risk factors
Risk for ERMs increases with age, and males and females are equally affected.
Both eyes have ERMs in 10-20% of cases.
Diagnostic testing
Most ERMs can be detected on a routine dilated eye exam.
An optical coherence tomography (OCT) is a noninvasive test that takes a picture of the back of the eye. It can detect and monitor the progression of the ERM over time.
Treatment and prognosis
Since most ERMs are asymptomatic, no treatment is necessary. However, if there is significant visual distortion from the ERM or significant progression of the membrane over time, then surgical intervention is recommended. There are no eye drops, medications, or nutritional supplements to treat or reverse an ERM.
The surgery is called a vitrectomy with membrane peeling. The vitrectomy removes the vitreous gel and replaces it with a saline solution. The epiretinal membrane is then peeled off the surface of the retina with forceps.
Surgery has a good success rate and patients in general have less distortion after surgery.
Article contributed by Dr. Jane Pan
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Do you have floaters in your vision?
Floaters are caused by thick areas in the gel-like fluid that fills the back cavity of your eye, called the vitreous.
Many people, especially highly near-sighted people, often see some degree of floaters for a good portion of their lives. Often, these floaters are in the periphery of your vision and may only be visible in certain lighting conditions. The most frequent conditions are when you are in bright sunlight and are looking toward the clear blue sky. This I know from personal experience as I have a floater in my left eye that I most often see when swimming outdoors. Every time I turn my head to the left to breathe I see this floater moving in my peripheral vision.
This is totally harmless other than when I’m swimming in the ocean and swear that sudden object in my peripheral vision is a shark bearing down on me. Some people who have floaters are not as lucky and the floater can be very central and almost constantly annoying, especially when trying to read.
The second scenario in which floaters occur is during the normal aging process. The vitreous gel in the back of the eye starts to shrink as we age and at some point it collapses in on itself and pulls away from the retina. This sometimes results in a sudden set of new floaters.
When that happens you need to be checked for signs of a retinal tear or detachment. As long as your retina survives that episode without any problems, the floaters themselves may stick around for a while and can be rather annoying.
Most people eventually adapt to the floaters; the brain learns to filter them out so you are no longer aware of them. The vitreous can also collapse more as time goes on and the dense floater you are seeing initially may move further forward and drop lower in the eye so the shadow it is casting is less intense and more in the periphery of your vision where it is much easier to ignore.
The first line of treatment for floaters has been, and still is, to live with them. Once you have your retina checked and there is nothing wrong there, the floaters themselves are harmless and will not lead to any further deterioration of your vision, which is why, if at all possible, you should just live with them. This is especially true if the floaters are new because the overwhelming majority of people with new floaters will eventually get to the point where they are no longer seeing them or at least where they are not interfering with normal daily activities.
If you have tried to wait them out and live with them but they are still interfering with your normal daily activities, you may want to consider having them treated with a laser.
This treatment is relatively new and involves using a special laser to try to break down large floaters into much smaller pieces that may no longer be visible. In a recent study of the laser treatment involving 52 patients, 36 were treated with the laser (a single laser treatment session) and 16 people had a sham treatment (meaning they went through everything the treated group did but did not actually have the real treatment done). In the people who were actually treated, 54% reported a significant improvement in the floater symptoms while 0% in the sham group reported any improvement (no placebo effect). There were no significant side effects in either group.
Some points to note in the above study:
Fifty-four percent of people treated noted a significant improvement in their floater symptoms with a single treatment. That’s clearly not anywhere near a guaranteed improvement.
Other people have noted an improvement after more than one session, bringing the total expected improvement into the 70% range, with one or more treatments.
Another point to note is that there were no significant side effects to the treatment.
Although true in this small study, it does not mean that there are no risks to the laser treatment. Although rare, there have been reports of damage to the retina, optic nerve, or the lens of the eye.
Another treatment that can be used to treat floaters is a surgical procedure called a vitrectomy. This involves surgically going inside the back of the eye and removing the vitreous. This surgical procedure carries a higher risk than the laser treatment and is not 100% effective.
In summary, this new laser treatment is a good addition to the tools to deal with significant floater problems. If you have floaters for at least six months and they are central and interfering with your normal daily activities such as reading or driving and you want to see if this laser treatment could be right for you, check with your eye doctor.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Have you ever wondered what happens to the visual system as we age? What does the term "second sight" mean? What is presbyopia? What are the eyes more susceptible to as the aging process occurs? What can be done to prevent certain aging factors of the eye? The answer lies in a theory known as apoptosis (no that's not the name of the latest pop artist).
Apoptosis is the pre-programmed life of every cell in our body. Most studies show that it's a function of our programmed DNA. It's the ability for cells to survive and thrive in the anatomical environment. The body's ability to withstand and thrive during the aging process depends on proper nutrition, good mental health, exercise, and adequate oxygen supply. That's why studies have shown smoking can shorten your life by a decade or more.
In regards to aging and the eye, there is a phenomina during the 6th to 7th decade of life called "second sight". This is simply progressive nearsightedness in older adults secondary to cataracts. Close to 50% of the population over 60 years old has cataracts. Cataracts are a clouding of the natural lens of the eye that can impair vision causing glare and loss of detail. When patients experience second sight, it is sometimes quite convenient for them: they see up close without the reading glasses they have been depended on since their 40s.
Another aspect of the aging process is losing your reading vision you had all your life. This is called Presbyopia. Presbyopia is a Latin term which means "old eyes."
What happens in Presbyopia?
Before our mid-forties, the natural lens of the eye is very pliable and can easily focus on items up close. But in our mid-forties, the lens tends to lose its elasticity. Whenexperiencing presbyopia, people generally hold reading material farther away to see it more clearly. Presbyopia can be managed through bifocal or multifocal glasses or contact lenses, and some surgeries.
As aging occurs, the eyes are more susceptible to cataracts, glaucoma, macular degeneration and vascular disorders of the eye as well as dry eye syndrome.
To help prevent and manage these conditions, there are a variety of options.
- Maintaining yearly dilated eye exams for preventative care.
- Protect your eyes against the sun with UV sunglasses.
- Take antioxidant vitamins to help bolster the protection of the macula.
- Use artificial tears to hydrate the eye and keep your body hydrated by drinking plenty of water.
- Keep emotional, physical, and mental stress to a minimum.
Being educated on how we age is the first steph towards good ocular health and diminished chances of early apoptosis.
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

The Centers for Disease Control estimates that more than 2.8 million people in the United States suffer a concussion -- or traumatic brain injury (TBI) -- every year, and vision can be affected.
The rate of childhood TBI visits to the emergency department more than doubled between 2001 and 2009, making children more likely than any other group to go to the ER with concussion symptoms.
It was once assumed that the hallmark of a concussion was a loss of consciousness. More recent evidence, however, does not support that. In fact, the majority of people diagnosed with a concussion do not experience any loss of consciousness. The most common immediate symptoms are amnesia and confusion.
There also are multiple visual symptoms that can occur with a concussion, either initially or during the recovery phase.
Visual symptoms after a concussion include:
-
Blurred vision.
-
Difficulty reading.
-
Double vision.
-
Light sensitivity.
-
Headaches accompanying visual tasks.
-
Loss of peripheral vision.
Most people with visual complaints after a concussion have 20/20 distance visual acuity so more specific testing of near acuity, convergence amplitudes, ocular motility, and peripheral vision must be done.
In a study done at the Minds Matter Concussion Program at the Children's Hospital of Philadelphia, patients with a concussion diagnosis underwent extensive vision testing, which assessed symptoms, visual acuity, eye alignment, near point of convergence, vergence amplitude and facility, accommodative amplitude and facility, and saccadic eye movement speed and accuracy.
A total of 72 children (mean age 14.6 years) were examined, and 49 (68%) of those were found to have one or more vision symptoms after concussion. The most common problems were convergence insufficiency (47.2%); accommodative insufficiency (33.3%); saccadic dysfunction (30.5%); and accommodative infacility (11.1%). The investigators also found that 64% of the children with convergence insufficiency also had an accommodative disorder.
Difficulties with accommodation and convergence make it very hard to read for any length of time, with blurring and fatigue and then loss of concentration occurring after a fairly short period of reading time.
For the majority of people suffering a mild to moderate TBI, most of these symptoms resolve in one to three weeks but in some they can persist much longer.
If your visual symptoms after a concussion persist past three weeks, a visit with an eye care specialist is recommended. There may be several options to help improve the symptoms with either prescription eyeglasses or prisms to assist the two eyes to focus together.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Did you know that having one's eyes tested can reveal symptoms of ADHD (Attention Deficit Hyperactivity Disorder)? ADHD is a set of symptoms that include trouble with focus, overactivity, and behavioral control. It is estimated that one in five people has some sort of ADHD.
ADHD is a condition that has multiple symptoms and it can affect any age, though commonly it affects children. There is difficulty with visual processing, which includes doubling letters, reversing letters, and jumping words and lines of print.
Eye examinations are a crucial part of the diagnosis of ADHD. Proper visual function can be assessed through a thorough eye exam. During the exam, visual complaints, focusing, and processing can be assessed to rule out ADHD.
When glasses are prescribed for an patient with ADHD, prescribing the correct type of lens is vital. Many patients benefit from an anti-glare/anti-reflective or AR treatment on their lenses. This cuts unnecessary light from entering the eye, making visual processing easier.
In some cases, it is discovered that the person has a non-ocular visual processing problem. This simply means that their eyes have little or nothing to do with the symptoms of ADHD. This gives valuable information to the health care provider that is managing the patient and suggests more non-ocular testing for a compete diagnosis.
ADHD is very common, and the great news is there are many treatment options. Many resources for help are available on the Internet and through health care channels.
Having an eye exam should be one of the first items on the checklist if you are suspicious about ADHD because valuable information on visual processing can be gained.
For more resources see these websites:
National Institute of Mental Health, www.nimh.nih.gov/
American Optometric Association, AOA.org
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
There are many options available to adults and children when it comes to wearing corrective lenses (glasses and contacts) when engaged in physical activities.
Here is a look at the different modalities and the pros and cons of each:
Prescription Sports Goggles (i.e. Rec Specs)
The main benefits of goggles when playing sports are stability of vision and eye protection. When playing fast-moving sports, like basketball, soccer, rugby, etc., elbows, wrists, and heads are flying around at high speed, increasing the risk of eye injury. The eyes and eye sockets can be protected when covered by shatter-proof lenses. Additionally, there is no worry of having a contact lens pop out of your eye, which can be a debilitating experience for some people. The main drawback to goggles is that they can be cumbersome, decrease peripheral vision, and fog up. Additionally, very high prescriptions might not be available due to frame limitations. On the whole, this is a very good option for many people. One additional advantage to sports goggles is that in many cases you can have the lens made out Transition glasses, so the lens darkens in sunlight and lightens as it gets darker.
Contact Lenses
Far and away the best option for actually seeing when playing sports is contact lenses, particularly soft contact lenses. The main benefits include full field of vision, no fogging of lenses, and obviously no unsightly, heavy glasses on your face. But where sports goggles shine, contact lenses fall short: higher risk of injury, possibly less stable vision (especially when wearing multifocal or astigmatic lenses), and the potential of a lens falling out during activities. With modern contact lenses, this rarely happens, however. Gas permeable (hard) lenses are not recommended for sports.
Wearing Nothing!
For those whose prescriptions are not so high as to prevent proper functioning without correction, wearing no correction whatsoever is a fine choice. I’m often asked by parents whether their child absolutely needs to wear correction when they are playing sports. The answer is, it depends on how high the prescription is and the activity in which the child is engaged. If someone can see well enough to perform tasks without being hindered, not wearing any correction is perfectly fine.
There are plenty of options available for athletes. Visit your eye doctor to see what the best option is for your particular needs.
Article contributed by Dr. Jonathan Gerard
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

