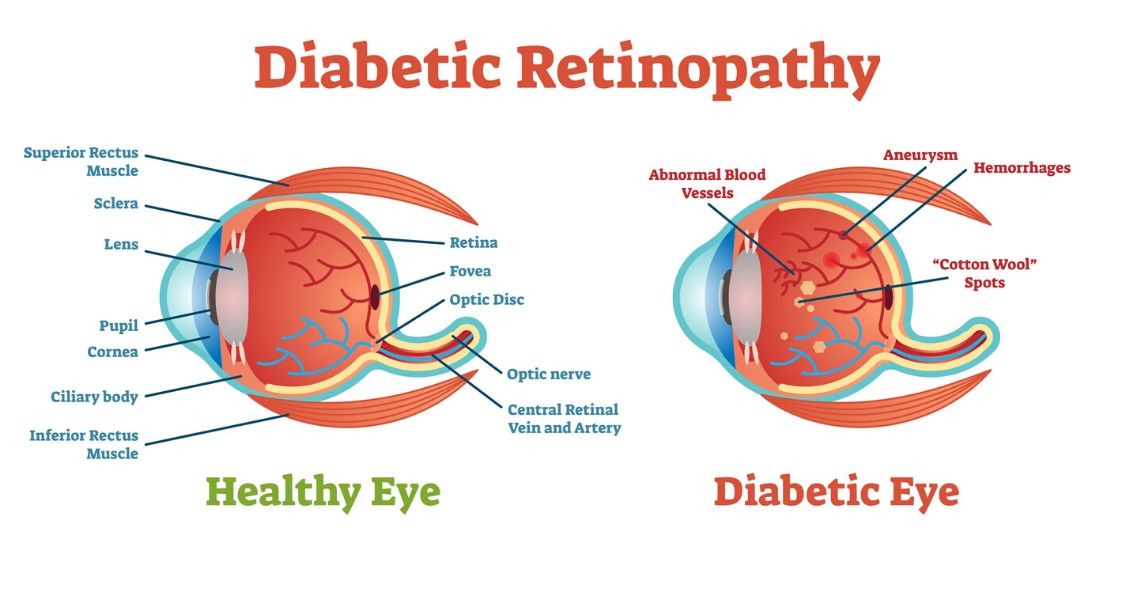
Diabetic retinopathy is an eye condition that can affect the retina of people who have diabetes.
The retina is the light-sensitive tissue that lines the back of the eye, and it detects light that is then processed as an image by the brain. Chronically high blood sugar or large fluctuations in blood sugar can damage the blood vessels in the retina. This can result in bleeding in the retina or leakage of fluid.
Diabetic retinopathy can be divided into non-proliferative or proliferative diabetic retinopathy.
Non-proliferative diabetic retinopathy: In the early stage of the disease, there is weakening of the blood vessels in the retina that causes out-pouching called microaneurysms. These microaneurysms can leak fluid into the retina. There can also be yellow deposits called hard exudates present in the retina from leaky vessels.
Diabetic macula edema is when the fluid leaks into the region of the retina called the macula. The macula is important for sharp, central vision needed for reading and driving. The accumulation of fluid in the macula causes blurry vision.
Proliferative diabetic retinopathy: As diabetic retinopathy progresses, new blood vessels grow on the surface of the retina. These blood vessels are fragile, which makes them likely to bleed into the vitreous, which is the clear gel that fills the middle of the eye. Bleeding inside the eye is seen as floaters or spots. Over time, scar tissue can then form on the surface of the retina and contract, leading to a retinal detachment. This is similar to wallpaper contracting and peeling away from the wall. If left untreated, retinal detachment can lead to loss of vision.
Symptoms of diabetic retinopathy:
- Asymptomatic: In the early stages of mild non-proliferative diabetic retinopathy, the person will usually have no visual complaints. Therefore, it is important for people with diabetes to have a comprehensive dilated exam by their eye doctor once a year.
- Floaters: This is usually from bleeding into the vitreous cavity from proliferative diabetic retinopathy.
- Blurred vision: This can be the result of fluid leaking into the retina, causing diabetic macular edema.
Risk factors for diabetic retinopathy:
- Blood sugar. Lower blood sugar will delay the onset and slow the progression of diabetic retinopathy. Chronically high blood sugar and the longer the duration of diabetes, the more likely chance of that person having diabetic retinopathy.
- Medical conditions. People with high blood pressure and high cholesterol are at greater risk for developing diabetic retinopathy.
- Ethnicity. Hispanics, African Americans and Native Americans are at greater risk for developing diabetic retinopathy.
- Pregnancy. Women with diabetes could have an increased risk of developing diabetic retinopathy during pregnancy. If they already have diabetic retinopathy, it might worsen during pregnancy.
Article contributed by Jane Pan M.D.
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ

There are certain eye conditions where an injection into your eye might be recommended.
Injections into the eye, specifically into the vitreous or gel-filled cavity of the eye, are called intravitreal injections.
In Part 1 of "You Want to Do WHAT to My Eye?" we talked mostly about anti-vascular endothelial growth factor (anti-VEGF) injections. Anti-VEGF injections are probably the most commonly injected agents and they are used to treat wet age-related macular degeneration (ARMD), diabetic retinopathy, and retinal vein occlusion.
But there are other injections that may be used as treatment.
Another injected medication used in combination with Anti-VEGF agents to treat wet macular degeneration, diabetic retinopathy and retinal vein occlusion are steroids. Additionally, steroids can be used to treat inflammation, or uveitis, in the eye. There is a steroid implant called Ozurdex, that looks like a white pellet and can last up to 3 months in the eye. The downside of steroids is that they can increase eye pressure and cause progression of cataracts.
Antibiotics are another type of medication that can be injected into the eye. Sometimes an infection called endophthalmitis can develop inside the eye. This can occur after eye surgery or a penetrating injury to the eye. The presenting signs and symptoms of endophthalmitis are loss of vision, eye pain and redness of the eye. Bacteria is usually the cause of the infection, and antibiotics are the treatment. The best way to deliver the antibiotics is to inject them directly into the eye.
Another relatively new injection is Jetrea, an enzyme that breaks down the vitreous adhesions that may develop on the surface of the retina. As we age, the vitreous contracts away from the retinal surface. When this occurs over the macula, the region responsible for fine vision, the result is visual distortion. Jetrea is an injection that will dissolve the vitreous adhesions and relieve the traction on the retina. Prior to the advent of Jetrea, the only treatment would have been surgery to physically remove the vitreous jelly and traction on the retina.
The next time you visit your eye doctor and are told you need an injection of medication, it will likely be one of the above agents.
Article contributed by Dr. Jane Pan

There are some eye conditions where your doctor might recommend an eye injection as a treatment option.
Injections into the eye, specifically into the vitreous or gel-filled cavity of the eye, are called intravitreal injections.
Anti-vascular endothelial growth factors (anti-VEGF) are probably the most commonly injected agents. They are used to treat wet age-related macular degeneration (ARMD), diabetic retinopathy, and retinal vein occlusion.
In these conditions, there are abnormal leaky blood vessels that cause fluid and blood to accumulate in and under the retina. This accumulation of fluid results in loss of central vision. The role of anti-VEGF agents is to shrink these abnormal vessels and restore the normal architecture of the retina.
There are three anti-VEGF agents widely administered: Lucentis, Avastin, and Eylea.
Lucentis (Ranibizumab) is FDA approved for treatment of wet ARMD, diabetic retinopathy, and vein occlusion. It is specially designed for injection into the eye and is a smaller molecule than Avastin so it may have better penetration into the retina.
Avastin (Bevacizumab) was originally approved by FDA for treating colorectal cancer. It is used “off-label” for the same treatment indications as Lucentis. Off-label usage of medication is legal, but pharmaceutical companies can't promote a medication for off-label use. The amount of Avastin needed for eye injections is a fraction of the amount used to treat colorectal cancer, therefore, the cost of ophthalmic Avastin is only a fraction of the cost of Lucentis. This means that Avastin needs to be prepared sterilely into smaller doses by an outside pharmacy prior to injection into the eye.
Eylea (Aflibercept) is the third anti-VEGF agent. It was designed to have more binding sites than Avastin and Lucentis so it may last longer in the eye than the former two. Eylea is FDA approved for treatment of wet ARMD, diabetic disease, and vein occlusion, and therefore, the cost of Eylea is similar to the cost of Lucentis.
Various studies have been performed to compare these agents. The most anticipated study was the CATT trial (N Engl J Med 2011; 364:1897-1908), which compared Avastin and Lucentis for the treatment of wet ARMD.
The study found that both had equivalent treatment effects on vision over the course of a year. In general, most ophthalmologists would consider all three agents to be very similar.
There is a thought that after prolonged injections, some patients may develop resistance to one particular agent but still respond to the other 2 agents. Therefore, your ophthalmologist will individualize your treatment.
Article contributed by Dr. Jane Pan

Fall brings a lot of fun, with Halloween bringing loads of it.
But did you know that some Halloween practices could harm your vision? Take Halloween contacts, for instance. They vary widely, with everything from monster eyes to goblin eyes to cat eyes to sci-fi or a glamour look. They can be just the added touch you need for that perfect costume. However, some people do not realize that the FDA classifies contact lenses as a medical device that can alter cells of the eye and that damage can occur if they are not fit properly.
Infection, redness, corneal ulcers, hypoxia (lack of oxygen to the eye) and permanent blindness can occur if the proper fit is not ensured. The ICE, FTC, and FDA are concerned about costume contacts from the illegal black market because they are often unsafe and unsanitary. Proper safety regulations are strictly adhered to by conventional contact lens companies to ensure that the contact lenses are sterile and packaged properly and accurately.
Health concerns arise whenever unregulated black-market contacts come into the US market and are sold at flea markets, thrift shops, beauty shops, malls, and convenience stores. These contacts are sold without a prescriber's prescription, and are illegal in the US. There have also been reports of damage to eyes because Halloween spook houses ask employees to share the same pair of Halloween contact lenses as they dress up for their roles.
So the take home message is, have a great time at Halloween, and enjoy the flare that decorative contacts can bring to your costume, but get them from a reputable venue and be fit by an eye care professional with a proper legal prescription. Don't gamble with your eyes for a night of Halloween fun!
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ
We all know that during pregnancy, a woman's body goes through a great deal of change hormonally and physiologically. But did you know her eyes change as well? Below are some of the most common effects pregnancy can have on the eye.
- Corneal changes. In some cases, pregnancy can cause the cornea, the front window of the eye, to change curvature and even swell, leading to shifts in glasses and contact lens prescriptions. In addition, changes in the chemistry of the tear film can lead to dry eyes and contact lens intolerance. It is for these reasons that it is generally not recommended to have any new contact lens fitting or new glasses prescription checks until several months postpartum. We want to get the most accurate measurements possible.
- Retinal changes. Many different conditions can affect the retina during pregnancy. If the pregnant woman has diabetes, diabetic eye disease can progress by 50%. In women with preeclampsia, a condition where blood pressure rises significantly, over 40% of women can show changes in the retinal blood vessels, and 25% to 50% complain of changes to their vision.
- Eye Pressure Fluctuation. Intraocular pressure (IOP) usually decreases during pregnancy. The exact mechanism causing this is unknown, but it is usually attributed to an increase of flow of intraocular fluid out of the eye. This is good news for pregnant women with glaucoma or high IOP. In fact, the drop in IOP is larger when you start with a high IOP compared to one in the normal range.
There are many more effects that pregnancy can have on the eye, but these are the most common. One other thing to keep in mind is that though the likelihood of any adverse effect is extremely low, we try not to use any diagnostic eye drops on pregnant patients during the eye exam. Unless there is a medical necessity to dilate the pupils or check IOP, it is a good rule of thumb to put off using drops until after the patient has given birth in order to protect the developing baby.

The American Academy of Ophthalmology has recommendations for how often adults need to get their eyes examined and those recommendations vary according to the level of risk you have for eye disease.
For people who are not at elevated risk the recommendations are:
- Baseline eye exam at age 40.
- Ages 40-54 every 2-4 years.
- Ages 55-64 every 1-3 years.
- Ages 65 and older every 1-2 years.
Those recommendations are just for people who have NO added risk factors. If you are diabetic or have a family history of certain eye diseases then you need exams more frequently.
As you can see, the guidelines recommend more frequent exams as you get older. Here are the TOP 4 REASONS why you need your eyes examined more frequently as you get older:
1. Glaucoma
Glaucoma is the second leading cause of blindness in the United States. It has no noticeable symptoms when it begins and the only way to detect glaucoma is through a thorough eye exam. Glaucoma gets more and more common as you get older. Your risk of glaucoma is less then 1% if you are under 50 and over 10% if you are 80 or over. The rates are higher for African Americans. Glaucoma can be treated but not cured. The earlier it is detected and treated, the better your chances for keeping your vision.
2. Macular Degeneration
Macular degeneration is the leading cause of blindness in the U.S. Like glaucoma, it gets more common as you age. It affects less than 2% of people under 70, rises to 10% in your 80s and can get as high as 50% in people in their 90s. The rates are highest in Caucasians. Macular degeneration can also be treated but not cured. Early intervention leads to better outcomes.
3. Cataracts
As in the cases above, cataracts get more common as you get older. If they live long enough, almost everyone will develop some degree of cataracts. In most people, cataracts develop slowly over many years and people may not recognize that their vision has changed. If your vision is slowly declining from cataracts and you are not aware of that change it can lead to you having more difficulty in performing life’s tasks. We get especially concerned about driving since statistics show that you are much more likely to get in a serious car accident if your vision is reduced. There is also evidence that people with reduced vision from cataracts have a higher rate of hip fractures from falls.
4. Dry Eyes
Dry eyes can affect anyone at any age but the incidence tends to be at its highest in post-menopausal women. Dry eyes can present with some fairly annoying symptoms (foreign body sensation in the eye, burning, intermittent blurriness). Sometimes there aren’t any symptoms but during an exam we can see the surface of the cornea drying out. Dry eye can lead to significant corneal problems and visual loss if it gets severe and is left untreated.
One of the most heart-breaking things we see in the office is the 75-year-old new patient who hasn’t had an eye exam in 10 years and he comes in because his vision “just isn’t right” and his family has noticed he sometimes bumps into things. On exam his eye pressures are through the roof and he is nearly blind from undetected glaucoma. And at that point there is no getting back the vision he has lost. If he had only come in several years earlier and just followed the guidelines, all this could have been prevented. Now he is going to have to live out the rest of his years struggling with severe vision loss.
DON’T LET THAT BE YOU!!!!!!
Article contributed by Dr. Brian Wnorowski, M.D.
Read more: Top 4 Reasons Every Older Adult Needs Regular Eye Exams
"What are these weird floating things I started seeing?"
The spots, strings, or cobwebs that drift in and out of your vision are called “floaters,” and they are more prominent if you’re looking against a white background.
These floaters are tiny clumps of material floating inside the vitreous (jelly-like substance) that fills the inside of your eye. Floaters cast a shadow on the retina, which is the inner lining of the back of the eye that relays images to the brain.
As you get older, the vitreous gel pulls away from the retina and the traction on the retina causes flashing lights. These flashes can then occur for months. Once the vitreous gel completely separates from the back wall of the eye, you then have a posterior vitreous detachment (PVD), which is a common cause of new onset of floaters.
This condition is more common in people who:
- Are nearsighted.
- Are aphakic (absence of the lens of the eye).
- Have past trauma to the eye.
- Have had inflammation in the eye.
When a posterior vitreous detachment occurs, there is a concern that it can cause a retinal tear.
Symptoms of a retinal tear include:
- Sudden increase in number of floaters that are persistent and don't resolve.
- Increase in flashes.
- A shadow covering your side vision, or a decrease in vision.
In general, posterior vitreous detachment is unlikely to progress to a retinal detachment. Only about 15 percent of people with PVD develop a retinal tear.
If left untreated, approximately 40 percent of people with a symptomatic retinal tear will progress into a retinal detachment – and a retinal detachment needs prompt treatment to prevent vision loss.
Generally, most people become accustomed to the floaters in their eyes.
Surgery can be performed to remove the vitreous gel but there is no guarantee that all the floaters will be removed. And for most people, the risk of surgery is greater than the nuisance that the floaters present.
Similarly, there is a laser procedure that breaks the floaters up into smaller pieces in hopes of making them less noticeable. However, this is not a recognized standard treatment and it is not widely practiced.
In general, the usual recommendation for floaters and PVD is observation by an eye care specialist.
Article contributed by Jane Pan M.D.
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ. This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician.

One of the hardest questions eye care professionals deal with every day is when to tell people who are having difficulty with their vision that they need to stop driving.
Giving up your driving privilege is one of the most difficult realities to come to terms with if you have a problem that leads to permanent visual decline.
The legal requirements vary from state to state. For example, in New Jersey the legal requirement to drive, based on vision, is 20/50 vision or better with best correction in one eye for a “pleasure” driving license. For a commercial driving license, the requirement is 20/40 vision or better in both eyes.
In some states there is also a requirement for a certain degree of visual field (the ability to see off to the sides).
According to the Insurance Institute for Highway Safety, the highest rate of motor vehicle deaths per mile driven is in the age group of 75 and older (yes, even higher than teenagers). Much of this increased rate could be attributable to declining vision. There are also other contributing factors such as slower reaction times and increased fragility but the fact remains that the rate is higher, so when vision problems begin to occur with aging it is extremely important to do what is necessary to try to keep your vision as good as possible.
That means regular eye exams, keeping your glasses prescription up-to-date, dealing with cataracts when appropriate, and staying on top of other vision-threatening conditions such as macular degeneration, glaucoma and diabetes.
It is our responsibility to inform you when you are no longer passing the legal requirement to drive. Although there is no mandatory reporting law in all states, it is recorded in your medical record that you were informed that your vision did not pass the state requirements to maintain your privilege. And, yes, it is a privilege -- not a right -- to drive.
If you have a significant visual problem and your vision is beginning to decline, you need to have a frank discussion with your eye doctor about your driving capability. If you are beginning to get close to failing the requirement you need to start preparing with family and loved ones about how you are going to deal with not being able to drive.
Many of us eye doctors have had the unfortunate occurrence of having instructed a patient to stop driving because of failing vision, only to have him ignore that advice and get in an accident. Don’t be that person. Be prepared, have a plan.
Article contributed by Dr. Brian Wnorowski, M.D.
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ. This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician.
Who is Charles Bonnet? He was a Swiss naturalist, philosopher, and biologist (1720-1793) who first described the hallucinatory experiences of his 89-year-old grandfather, who was nearly blind in both eyes from cataracts. Charles Bonnet Syndrome is now the term used to describe simple or complex hallucinations in people who have impaired vision.
Symptoms
People who experience these hallucinations know they aren't real. These hallucinations are only visual, and they don't involve any other senses. These images can be simple patterns or more complex, like faces or cartoons. They are more common in people who have retinal conditions that impair their vision, like macular degeneration, but they can occur with any condition that damages the visual pathway. The prevalence of Charles Bonnet Syndrome among adults 65 years and older with significant vision loss is reported to be between 10% and 40%. This condition is probably under reported because people may be worried about being labeled as having a psychiatric condition.
Causes
The causes of these hallucinations are controversial, but the most supported theory is deafferentation, which is the loss of signals from the eye to the brain; then, in turn, the visual areas of the brain discharge neural signals to create images to fill the void. This is similar to the phantom limb syndrome, when a person feels pain where a limb was once present. In general, the images that are produced by the brain are usually pleasant and non-threatening.
Treatment and prognosis
If there is a reversible cause of decreased vision, such as significant cataract, then once the decreased vision is treated, the hallucinations should stop.
There is no proven treatment for the hallucinations as a result of permanent vision loss but there are some techniques to manage the condition. Give these a try if you have Charles Bonnet Syndrome.
- Talking about the hallucinations and understanding that it is not due to mental illness can be reassuring.
- Changing the environment or lighting conditions. If you are in a dimly lit area, then switch on the light and vice versa.
- Blinking and moving your eyes to the left and right and looking around without moving your head have been reported as helpful.
- Resting and relaxing. The hallucinations may be worse if you are tired or sick.
- Taking antidepressants and anticonvulsants have been used but have questionable efficacy.
Over time, the hallucinations become more manageable and can decrease or even stop after a couple of years.
If you experience any of these symptoms, please get evaluated by your eye doctor to make sure there is not a treatable eye condition. Don’t be embarrassed or ashamed—your issue is likely caused by a physical disturbance and we are here to help!
Article contributed by Jane Pan
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Read more: Visual Hallucinations? It Could Be Charles Bonnet Syndrome.
Alzheimer's Disease International estimates that the number of people living with dementia worldwide - nearly 44 million in 2014 - will almost double by 2030 and more than triple by 2050.
There is no single test that can show if a person has Alzheimer's, but doctors can almost always determine if a person has dementia, although it may be difficult to determine the exact cause. Diagnosing Alzheimer's requires careful medical evaluation, neurological testing, and sometimes brain imaging and blood tests to rule out other causes of dementia.
Most of the testing for early disease - MRI scans of the brain, brain PET scans looking for amyloid, and spinal taps looking for certain proteins in the spinal fluid - are not very accurate, and they are invasive and often expensive.
Researchers have now turned to findings in the eye to help with early detection and are hoping to find ways to make the diagnosis earlier when potential treatments may have a better outcome. There is also hope that these tests will be less expensive and invasive then the other options.
One of the tests that has shown promise is an OCT of the retina. Almost every eye doctor’s office already has an OCT, and so if this research proves fruitful, the test could be done relatively cheaply because there is not a need to buy more expensive equipment. Right now, the average OCT exam is reimbursed at about the $50 per exam level, much less than the cost of an MRI or PET Scan.
Neuroscientists at the Gladstone Institutes in San Francisco showed a proof of concept in frontotemporal dementia, which is like Alzheimer’s but attacks much earlier and accounts for just 10% to 15% of dementia cases. They found that patients with frontotemporal dementia had thinning of the neuron layer of the retina on OCT.
In a study at Moorfields Eye Hospital they also found that people who had a thinner layer of neurons in the macula on an OCT exam were more likely to perform poorly on the cognitive tests - a clear warning sign they may be undergoing the early stages of dementia.
Study leader Dr. Fang Ko, said: “Our findings show a clear association between thinner macular retinal nerve fiber layer and poor cognition in the study population. This provides a possible new biomarker for studies of neurodegeneration.”
A second marker that is getting a careful look is identifying the presence of amyloid in the eye. Amyloid, thought to be one of the key causes of Alzheimer’s, which makes up most dementia cases, is often found to have formed into clumps and plaques in the brain. Scientists at Waterloo University in Canada found people with severe Alzheimer’s disease had deposits of a protein amyloid on their retinas.
Research conducted at Lifespan-Rhode Island Hospital in Providence co-led by Peter Snyder, a professor of neurology at Brown University, and Cláudia Santos, a graduate student at the University of Rhode Island, is attempting to detect amyloid in the retina by OCT and follows people over time to see if the amyloid increases and if it correlates with cognitive impairment.
Another angle being pursued by a company called Cognoptix is looking for amyloid in the lens of the eye. Using Cognoptix's SAPPHIRE II system, which detects amyloid in the lens, a 40-person Phase 2 clinical trial was conducted at four sites. The study recruited patients who were clinically diagnosed with probable Alzheimer’s disease (AD) via a rigorous neuropsychological and imaging workup. The study, using age-matched healthy controls, showed outstanding results of 85% sensitivity, and 95% specificity in predicting which people had probable AD.
The company is now planning a Phase 3 study that must show a strong correlation in a bigger study group to obtain ultimate FDA approval.
One of the other items I was going to include in this post was information on what visual symptoms occur in dementia patients and how family and friends can support them but I found an outstanding review already available online by the Alzheimer’s society that covers all those points. If you have a loved one with dementia this is an excellent read and I highly recommend you take the time to review it.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Eye drops can be hard for some patients to put into their eyes. After cataract surgery, there are two main issues we are trying to control: Preventing infection and controlling inflammation. Traditionally, we prescribed antibiotic eye drops to prevent infection, as well as steroid eye drops to control post-operative inflammation. Now we have some alternatives to using eye drops after surgery.
There are some antibiotic solutions we can place inside the eye at the end of the cataract surgery that have been shown in most studies to do as good or better a job preventing infection as using antibiotic eye drops before and after surgery.
Just recently, the FDA approved two new steroid delivery methods to reduce post-operative inflammation that have the potential to eliminate post-op steroid eye drops in most (but not all) patients who are undergoing cataract surgery. Those two products are called Dexycu and Dextenza.
Dexycu is a white bolus of steroid medication that is injected inside the eye after cataract surgery. It will not be visible in most patients because it is injected behind the iris, or the colored part of the eye. It sometimes doesn’t stay behind the iris and you might see a small white dot in the eye initially after surgery. It is a sustained-released medication, is resorbed over a couple of weeks and replaces the need for post-operative steroid drops.
Dextenza is a white pellet that is inserted into the lower punctum of the lid, which is the small opening for the drainage of tears. This insert is designed to deliver medication for up to 30 days. It is slowly resorbed and doesn't need to be removed. Similarly, it is usually not visible and does not cause any discomfort.
If you have either a Dexycu or Dextenza implant placed and an antibiotic medication is injected inside the eye after surgery, then you may be drop free after surgery. The main difference between the two steroid injections is that Dexycu is injected inside the eye while Dextenza is deposited outside the eye. For each of these new options there is a chance that in your particular case there may still be too much inflammation and you might need to take eye drops for a while, but the majority of the time you would not need drops.
If you are going to have cataract surgery and would like to be drop free after the procedure, then ask your surgeon if you would be a candidate for either the Dexycu or Dextenza implant.
Article contributed by Dr. Jane Pan.
"What are these weird floating things I started seeing?"
The spots, strings, or cobwebs that drift in and out of your vision are called “floaters,” and they are more prominent if you’re looking against a white background.
These floaters are tiny clumps of material floating inside the vitreous (jelly-like substance) that fills the inside of your eye. Floaters cast a shadow on the retina, which is the inner lining of the back of the eye that relays images to the brain.
As you get older, the vitreous gel pulls away from the retina and the traction on the retina causes flashing lights. These flashes can then occur for months. Once the vitreous gel completely separates from the back wall of the eye, you then have a posterior vitreous detachment (PVD), which is a common cause of new onset of floaters.
This condition is more common in people who:
- Are nearsighted.
- Are aphakic (absence of the lens of the eye).
- Have past trauma to the eye.
- Have had inflammation in the eye.
When a posterior vitreous detachment occurs, there is a concern that it can cause a retinal tear.
Symptoms of a retinal tear include:
- Sudden increase in number of floaters that are persistent and don't resolve.
- Increase in flashes.
- A shadow covering your side vision, or a decrease in vision.
In general, posterior vitreous detachment is unlikely to progress to a retinal detachment. Only about 15 percent of people with PVD develop a retinal tear.
If left untreated, approximately 40 percent of people with a symptomatic retinal tear will progress into a retinal detachment – and a retinal detachment needs prompt treatment to prevent vision loss.
Generally, most people become accustomed to the floaters in their eyes.
Surgery can be performed to remove the vitreous gel but there is no guarantee that all the floaters will be removed. And for most people, the risk of surgery is greater than the nuisance that the floaters present.
Similarly, there is a laser procedure that breaks the floaters up into smaller pieces in hopes of making them less noticeable. However, this is not a recognized standard treatment and it is not widely practiced.
In general, the usual recommendation for floaters and PVD is observation by an eye care specialist.
Article contributed by Jane Pan M.D.
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ. This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician.
The majority of cataract surgeries performed in the U.S. are done with a local anesthetic and IV sedation.
The local anesthesia may be accomplished in one of two ways: either an injection of anesthetic around the eye or anesthetic eye drops placed on the eye, often combined with an injection of a small amount of anesthetic into the front of the eye at the very beginning of surgery.
The injection of anesthetic around the eye generally produces a deeper anesthesia for the surgery than the topical method but it also comes with increased risk. There is a very small chance of potentially serious bleeding behind the eye and a rare chance of inadvertent penetration of the back of the eye with the injection needle.
The topical anesthesia has lower risk but does not provide quite as deep of an anesthesia, although the overwhelming majority of people having cataract surgery with a topical anesthetic do not experience any significant pain during the procedure.
The other difference between the two anesthesias is with that topical anesthesia you maintain your ability to move your eye around whereas with injection anesthesia the eye muscles are temporarily paralyzed so your eye doesn’t move during the surgery. When you have topical anesthesia it is important for you to try to stare straight ahead at the light in the microscope above you. Most people accomplish this quite easily.
Along with the anesthetic to the eye, in most cataract surgeries an anesthetist will also give you some mild sedative medication through an IV. This relaxes you but does not put you “out,” although some people do fall asleep during the procedure from the effects of the sedation.
Many people who have cataract surgery with IV sedation don’t remember some of the surgery because of the amnesiac effect that occurs from the sedative. This often doesn’t happen when you return for surgery on your second eye.
Despite often getting the exact same dose of sedative on the second surgery you have significant less amnesia the second time. This is caused by a quick buildup in tolerance to the medication.
When they have their second surgery, many patients feel that the surgery was significantly different than the first time even though it was done exactly the same. The reason is just that you remember more the second time.
On rare occasions people need to have general anesthesia to have their cataracts removed. Today, that is mostly done for people who are incapable of cooperating and staying still for the surgery. For everyone who can cooperate it is generally not worth the risks, which include death, to put people to sleep for a surgery that is easily done under a local anesthetic.
Article contributed by Dr. Brian Wnorowski, M.D.
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ
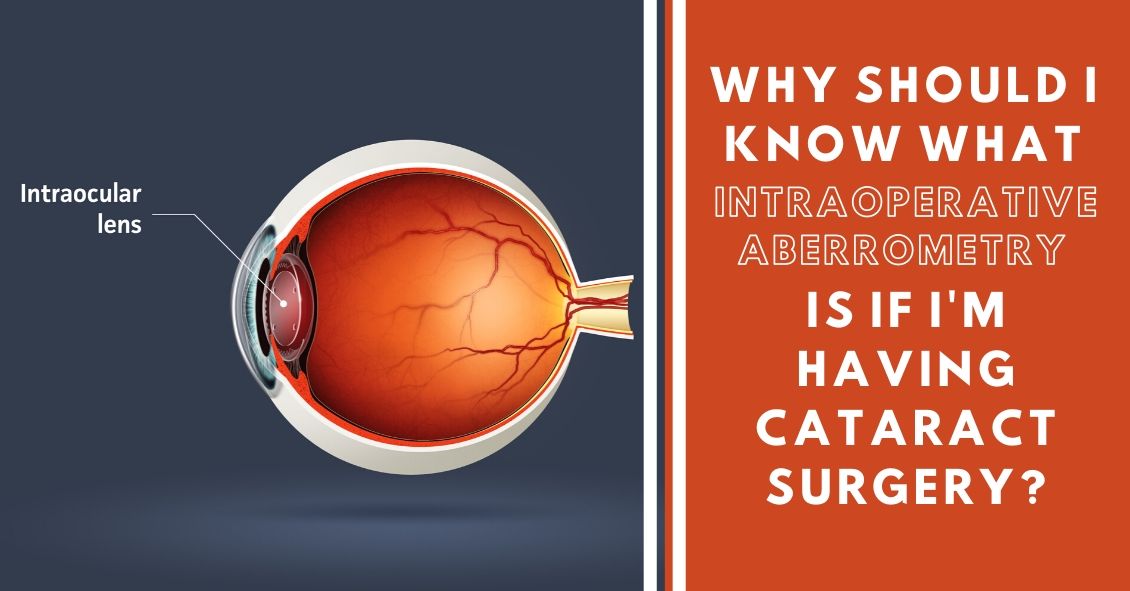
What Is Intraoperative Aberrometry?
Yes, that is a mouthful, but the concept isn’t quite as hard as the name.
An Intraoperative Aberrometer is an instrument we can use in the operating room to help us determine the correct power of the implant we put in your eye during cataract surgery.
Cataract surgery is the removal of the cloudy natural lens of your eye and the insertion of a new artificial lens inside your eye called an intraocular lens (IOL).
The cloudy cataract that we are removing has focusing power (think of a lens in a camera) and when that lens is removed, we need to insert an artificial lens in its place to replace that focusing power. The amount of focusing power the new IOL needs has to match the shape and curvature of your eye.
To determine what power of lens we select to put in your eye, we need to measure the shape and curvature of your eye prior to surgery. Once we get those measurements, we can plug those numbers into several different formulas to try and get the most accurate prediction of what power lens you need.
Overall, those measurements and formulas are very good at accurately predicting what power lens you should have. There are, however, several eye types where those measurements and formulas are less accurate at predicting the proper power of the replacement lens.
Long Eyes: People who are very nearsighted usually have eyes that are much longer than average. This adds some difficulty with the accuracy of both the measurements and the formulas. There are special formulas for long eyes but even those are less accurate than formulas for normal length eyes.
Short Eyes: People who are significantly farsighted tend to have shorter-than-normal eyes. Basically, the same issues hold true for them as the ones for longer eyes noted above.
Eyes with previous refractive surgery (LASIK, PRK, RK): These surgeries all change the normal shape of the cornea. This makes the formulas we use on eyes that have not had previous surgery not work as well when the normal shape of the cornea has been altered.
This is where intraoperative aberrometry comes in. The machine takes the measurements that we do before surgery and then remeasures the eye while you are on the operating room table after the cataract is removed and before the new implant is placed inside the eye. It then presents the surgeon with the power of the implant that the aberrometer thinks is the correct one. Unfortunately, the power that the aberrometer isn’t always exactly right, but with the combination of the pre-surgery measurements and the intra-surgery measurements the overall accuracy is significantly enhanced.
The intraoperative aberrometry is also very helpful in choosing the power of specialty lenses like multi-focal and toric lenses.
We would encourage you to consider adding intraoperative aberrometry to your cataract surgery procedure if you have either a long or short eye (usually manifested as a high prescription in your glasses) or if you have had any previous refractive surgery.
Article contributed by Dr. Brian Wnorowski, M.D.
Read more: Intraoperative Aberrometry & Cataract Lens Replacement Selection

What do Amblyopia, Strabismus, and Convergence Insufficiency all have in common? These are all serious and relatively common eye conditions that children can have.
Did you know that 80% of learning comes through vision? The proverb that states ”A picture is worth a thousand words” is true! If a child has a hard time seeing, it stand to reason that she will have a hard time learning.
Let’s explore Amblyopia, or “lazy eye”. It affects 3-5% of the population, enough that the federal government funded children’s yearly eye exams into the Accountable Care Act or ObamaCare health initiative. Amblyopia occurs when the anatomical structure of the eye is normal but the “brain-eye connection” is malfunctioning. In other words, it is like plugging your computer into the outlet but the power cord is faulty.
Amblyopia need to be caught early in life--in fact if it is not caught and treated early (before age 8) it can lead to permanent vision impairment. Correction with glasses or contacts and patching the good eye are ways it is treated. Most eye doctors agree that the first exam should take place in the first year of life. Early detection is a key.
Strabismus is a condition that causes an eye to turn in (esotropia), out (exotropia), or vertically. It can be treated with glasses or contacts, and surgery, if needed. Vision therapy or strategic eye exercises prescribed by a doctor can also improve this condition.
When we read, our brain tells our eyes to turn in to a comfortable reading posture. In Convergence Insufficiency, the brain tells the eyes to turn in, but they instead turn out, causing tremendous strain on that child’s eye for reading. Another tell tale sign of this condition is the inability to cross your eyes when a target approaches. The practitioner will see instead, that one of the eyes kicks out as the near target approaches. This condition can be treated with reading glasses or contacts, and eye exercises that teach the muscles of the eye to align properly during reading. Vision therapy is the treatment of choice for Convergence Insufficiency.
It is important to understand the pediatric eye and all the treatments that can be implemented to augment the learning process. Preventative care in the form of early eye examinations can mean the difference between learning normall or struggling badly. Remember, a young child can’t tell you if he hasa vision impairment. For the success of the child, be proactive by scheduling an early vision exam.
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Have you ever seen a temporary black spot in your vision? How about jagged white lines? Something that looks like heat waves shimmering in your peripheral vision?
If you have, you may have been experiencing what is known as an ocular migraine. Ocular migraines occur when blood vessels spasm in the visual center of the brain (the occipital lobe) or the retina.
They can take on several different symptoms but typically last from a few minutes to an hour. They can take on either positive or negative visual symptoms, meaning they can produce what looks like a black blocked-out area in your vision (negative symptom), or they can produce visual symptoms that you see but know aren’t really there, like heat waves or jagged white lines that look almost like lightning streaks (positive symptoms).
Some people do get a headache after the visual symptoms but most do not. They get the visual symptoms, which resolve on their own in under an hour, and then generally just feel slightly out of sorts after the episode but don’t get a significant headache. The majority of episodes last about 20 minutes but can go on for an hour. The hallmark of this problem is that once the visual phenomenon resolves the vision returns completely back to normal with no residual change or defect.
If you have this happen for the first time it can be scary and it is a good idea to have a thorough eye exam by your eye doctor soon after the episode to be sure there is nothing else causing the problem.
Many people who get ocular migraines tend to have them occur in clusters. They will have three or four episodes within a week and then may not have another one for several months or even years.
There are some characteristics that raise your risk for ocular migraines. The biggest one is a personal history of having migraine headaches. Having a family history of migraines also raises your risk, as does a history of motion sickness.
Although the symptoms can cause a great deal of anxiety, especially on the first occurrence, ocular migraines rarely cause any long-term problems and almost never require treatment as long as they are not accompanied by significant headaches.
So if symptoms like this suddenly occur in your vision, try to remain calm, pull over if you are driving, and wait for them to go away. If they persist for longer than an hour, you should seek immediate medical attention.
Article contributed by Dr. Brian Wnorowski, M.D.
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ
When your eyes feel itchy, it’s a natural reaction to want to rub, rub, rub. It temporarily relieves the itching, and frankly feels great when you’re doing it. Unknowingly, however, you are likely doing short-term – and in some cases long-term – damage to your eyes. Here are some of the detrimental effects that can result from eye rubbing.
- Worsening of ocular allergies: rubbing an eye inflamed from allergies starts a vicious cycle. During the allergic ocular response, a chemical called histamine is released from a cell called a mast cell. It is this release of histamine that starts the red, itchy, watery eyes associated with allergies. Rubbing the eyes releases more histamine, causing the eyes to become more inflamed, perpetuating the cycle.
- Risk of increased eye pressure: Putting pressure on the globe of the eye drastically increases intraocular pressure (IOP). While the effect is temporary, prolonged rubbing can increase your risk of developing glaucoma, a potentially blinding eye disease, especially if the IOP spikes high enough.
- Risk of retinal detachment: Any trauma to the eye can risk detaching the retina, the paper thin film that lines the back of the eye. Retinal detachment can present with symptoms such as seeing flashes, floaters, or a blacking out of the vision, but other times it can go undetected until it’s too late. Rubbing the eye causes unnecessary trauma to the globe, which can rupture the attachment of the retina to the back of the eye.
- Keratoconus: More and more research is starting to show that ocular allergies and eye rubbing is a risk factor for developing keratoconus, a disease in which the cornea starts to bow out and form a cone shape. While the exact cause is not known, research suggests that the contant rubbing weakens the collagen bonds that helps the cornea keep its shape, resulting in the abnormal corneal bowing.
Nothing good comes from eye rubbing. If your eyes are itchy, you can try over-the-counter antihistamine drops, cool compresses (which slows histamine release), and allergy medications to stop the itch.
Article contributed by Jonathan Gerard
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ
Eye doctors typically pride themselves on being able to improve someone’s vision through glasses or contact lens prescriptions. Whether it’s a first-time glasses wearer, or someone having either a small or large change in their prescription, we like to aim for that goal of 20/20 vision.
Despite our best efforts, however, correcting vision to 20/20 is not always a positive outcome for the patient. Whether someone will be able to tolerate their new prescription is based on something called neuroplasticity, which is what allows our brains to adapt to changes in our vision.
You or someone you know may have had this happen: Your vision is blurry, so you go to the eye doctor. The doctor improves the vision, but when you get your new glasses, things seem “off.”
Common complaints are that the prescription feels too strong (or even too clear!) or that the wearer feels dizzy or faint. This is especially true with older patients who have had large changes in prescription, since neuroplasticity decreases with age. It is also more likely to happen when the new prescription has a change in the strength or the angle of astigmatism correction. Conversely, this happens less often in children, since their brains have a high amount of plasticity.
Quite often, giving the brain enough time to adapt to the new vision will decrease these symptoms.
Whenever a patient has a large change in prescription, I tell them that they should wear the glasses full time for at least one week. This is true for both large changes in prescription strength, as well as changing lens modality, i.e. single vision to progressives.
Despite the patient’s best efforts, though, sometimes allowing time to adapt to the new vision isn’t enough, and the prescription needs to be adjusted. Even when someone sees 20/20 on the eye chart with their new glasses, if they are uncomfortable in them even after trying to adjust for a week then we sometimes have to make a compromise and move the script back closer to their previous script so that there is less change and they can more easily adapt.
In conclusion, adapting to a new prescription can sometimes be frustrating. It does not mean there is anything wrong with you if you have difficulty adjusting to large changes in a prescription. With a little patience and understanding about how your brain adapts to these kinds of changes, your likelihood of success will be that much higher.
Article contributed by Dr. Jonathan Gerard
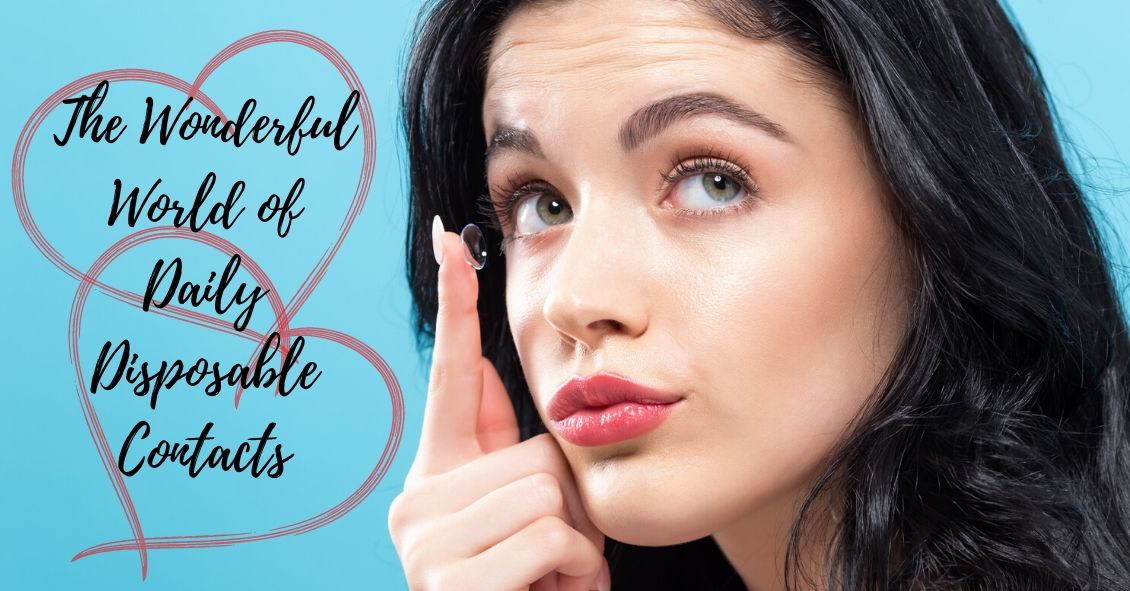
When soft contact lenses first came on the scene, the ocular community went wild.
People no longer had to put up with the initial discomfort of hard lenses, and a more frequent replacement schedule surely meant better overall health for the eye, right?
In many cases this was so. The first soft lenses were made of a material called HEMA, a plastic-like polymer that made the lenses very soft and comfortable. The downside to this material was that it didn’t allow very much oxygen to the cornea (significantly less than the hard lenses), which bred a different line of health risks to the eye.
As contact lens companies tried to deal with these new issues, they started to create frequent-replacement lenses that made from SiHy, or silicone hydrogel. The oxygen transmission problem was solved, but an interesting new phenomenon occurred.
Because these were supposed to be the “healthiest” lenses ever created, many people started to over wear their lenses, which led to inflamed, red, itchy eyes; corneal ulcers; and hypoxia (lack of oxygen) from sleeping in lenses at night. A new solution was needed.
Thus was born the daily disposable contact lens, which is now the go-to lens recommendation of most eye care practitioners.
Daily disposables (dailies) are for one-time use, and therefore there is negligible risk of over wear, lack of oxygen, or any other negative effect that extended wear (2-week or monthly) contacts can potentially have. While up-front costs of dailies are higher than their counterparts, there are significant savings in terms of manufacturer rebates. In addition, buying contact lens solution is no longer necessary!
While a very small minority of patient prescriptions are not yet available in dailies, the majority are, and these contacts have worked wonders for patients who have failed in other contacts, especially those who have dry eyes.
Ask your eye care professional how dailies might be the right fit for you.
Article contributed by Dr. Jonathan Gerard
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Sunglasses are more than just a fashion statement - they’re important protection from the hazards of UV light.
If you wear sunglasses mostly for fashion that’s great--just make sure the lenses block UVA and UVB rays.
And if you don’t wear sunglasses, it’s time to start.
Here are your top 6 reasons for wearing sunglasses:
Preventing Skin Cancer
One huge way that sunglasses provide a medical benefit is in the prevention of skin cancer on your eyelids. UV light exposure from the sun is one of the strongest risk factors for the development of skin cancers.
Each year there are more new cases of skin cancer than the combined incidence of cancers of the breast, prostate, lung and colon.
About 90 percent of non-melanoma skin cancers are associated with exposure to ultraviolet (UV) radiation from the sun.
Your eyelids, especially the lower eyelids, are also susceptible to UV light and they do develop skin cancers somewhat frequently.
Many people who now regularly apply sunscreen to help protect them from UV light often don’t get that sunscreen up to the edge of their eyelids because they know the sunscreen is going to make their eyes sting and burn. Unfortunately, that leaves the eyelids unprotected. You can fix that by wearing sunglasses that block both UVA and UVB rays.
Decreasing Risk For Eye Disease
There is mounting evidence that lifetime exposure to UV light can increase your risk of cataracts and macular degeneration. It also increases your risk of getting growths on the surface of your eye called Pinguecula and Pterygiums. Besides looking unsightly, these growths can interfere with your vision and require surgery to remove them.
Preventing Snow Blindness
Snow reflects UV light and on a sunny day the glare can be intense enough to cause a burn on your corne--much like what happens when people are exposed to a bright welding arc.
Protection From Wind, Dust, Sand
Many times, when you are spending time outdoors and it is windy, you risk wind-blown particles getting into your eyes. Sunglasses help protect you from that exposure. The wind itself can also make your tears evaporate more quickly, causing the surface of your eye to dry out and become irritated, which in turn causes the eye to tear up again.
Decreasing Headaches
People can get headaches if they are light sensitive and don’t protect their eyes from bright sunlight. You can also bring on a muscle tension headache if you are constantly squinting because the sunlight is too bright.
Clearer Vision When Driving
We have all experienced an episode of driving, coming around a turn, looking directly into the direction of the setting or rising sun, and having difficulty seeing well enough to drive. Having sunglasses on whenever you are driving in sunlight helps prevent those instances. Just a general reduction in the glare and reflections that sunlight causes will make you a better and more comfortable driver.
So it’s time to go out there and find yourself a good pair of sunglasses that you look great in and that protect your health, too.
Your eye-care professional can help recommend sunglasses that are right for your needs.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Fireworks Eye Injuries Have More Than Doubled in Recent Years
Fireworks sales will be blazing across the country from now through the Fourth of July. As retailers begin their promotions, the American Academy of Ophthalmology is shining a light on this explosive fact: The number of eye injuries caused by fireworks has more than doubled in recent years.
Fireworks injuries cause approximately 10,000 emergency room visits each year, according to data from the U.S. Consumer Product Safety Commission. The injuries largely occurred in the weeks before and after the Fourth of July. The CPSC’s most recent fireworks report showed that about 1,300 eye injuries related to fireworks were treated in U.S. emergency rooms in 2014, up from 600 reported in 2011.
To help prevent these injuries, the Academy is addressing four important things about consumer fireworks risks:
- Small doesn’t equal safe. A common culprit of injuries are the fireworks often handed to small children – the classic sparkler. Many people mistakenly believe sparklers are harmless due to their size and the fact they don’t explode. However, they can reach temperatures of up to 2,000 degrees – hot enough to melt certain metals.
- Even though it looks like a dud, it may not act like one. At age 16, Jameson Lamb was hit square in the eye with a Roman candle that he thought had been extinguished. Now 20, Lamb has gone through multiple surgeries, including a corneal transplant and a stem cell transplant.
- Just because you’re not lighting or throwing it doesn’t mean you’re out of the firing line. An international study of fireworks-related eye injuries showed that half of those hurt were bystanders. The researchers also found that one in six of these injuries caused severe vision loss.
- The Fourth can be complete without using consumer fireworks. The Academy advises that the safest way to view fireworks is to watch a professional show where experts are controlling the displays.
If you experience a fireworks eye injury:
- Seek medical attention immediately.
- Avoid rubbing or rinsing the eyes or applying pressure.
- Do not remove any object from the eye, apply ointments, or take any pain medications before seeking medical help.
Watch the AAO’s animated public service announcement titled “Fireworks: The Blinding Truth.”
Article contributed by Dr. Brian Wnorowski, M.D.
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ

