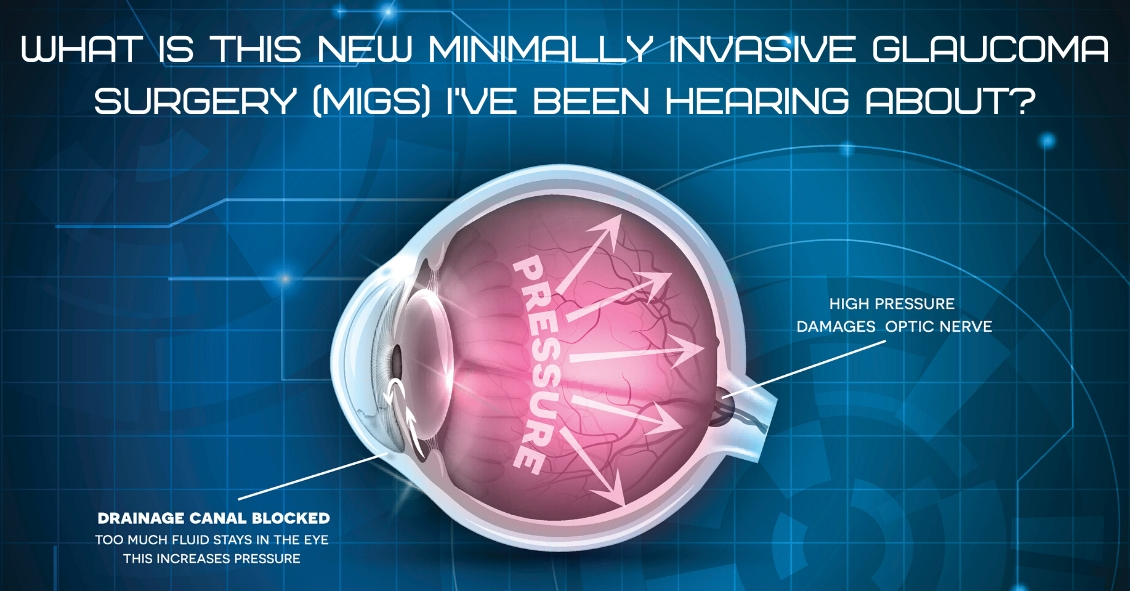
For over 40 years the standard surgical treatment for glaucoma was a procedure called a trabeculectomy.
In a trabeculectomy the ophthalmic surgeon would make a hole in the wall of eye to allow fluid from the inside of the eye to flow out of the eye and then get resorbed by the blood vessels in the conjunctiva (the mucous membrane that covers the white part of the eye).
This surgery often resulted in a large decrease in the Intraocular Pressure (IOP). Reducing the IOP is the goal of glaucoma surgery because multiple studies on glaucoma show that if you can reduce the pressure in glaucoma the progression of the disease slows.
The problem with trabeculectomy is although it frequently lowers the pressure it also has a fairly high complication and/or failure rate. This led to some reluctance to perform the procedure unless the glaucoma was severe, or the pressure was very high. As a result of those issues there has been a search during the last 40 years for something that had a lower complication rate and could be more easily deployed earlier in the disease process.
Enter Minimally Invasive Glaucoma Surgery, or MIGS. There are now several types of surgeries that fit in the MIGS category and many of them are used in conjunction with cataract surgery. They are utilized much earlier in the disease process and when combined with cataract surgery they can be used to not only help control the pressure over the long term but can often even reduce the burden of eye drops afterward.
The biggest advantage to MIGS over the trabeculectomy is that when used in conjunction with cataract surgery MIGS can lower the eye pressure (although not as much as the trabeculectomy) but often with no higher rate of complications as there is with cataract surgery alone.
The lower complication rate is mainly because the MIGS procedures do not create a full-thickness hole in the wall of the eye. Most of them involve putting in some form of stent inside the eye. The stent lets the intraocular fluid get out of the eye more efficiently through its normal internal drain called the trabecular meshwork, rather than having to flow to the outside of the eye as with a trabeculectomy. There are currently several FDA-approved drainage stents with more on the horizon.
A stent is not the only way to lower the pressure along with cataract surgery. There is also a laser treatment you can do from the inside of the eye that slows the amount of fluid the eye makes, which also results in a lower pressure. It is called Endocyclophotocoagulation (ECP). Think of a partially clogged drain in a sink with constantly running water. If you don’t want the sink to overflow (or the pressure in the eye to get too high) you either try to unclog the drain (stent) or you turn down the faucet (ECP).
MIGS has been a great development over the last several years, enabling the ophthalmic surgeon to intervene surgically at a much earlier stage of glaucoma and with a significantly lower complication rate than the more invasive trabeculectomy.
At this point I utilize one of the MIGS procedures in almost all patients who need their cataracts removed and are on one or more glaucoma medications. Even if the glaucoma is fairly well controlled at the time, the MIGS procedure gives us the opportunity to try and get a glaucoma patient off their eye drops, which is both a decreased burden of treatment and lets us keep the eye drops in reserve should the pressure start to increase again later in life.
If you have glaucoma and a cataract you should definitely discuss this with your doctor to see if a MIGS procedure along with your cataract surgery could be the right choice for you.
Article contributed by Dr. Brian Wnorowski, M.D.

1. Vision is so important to humans that almost half of your brain’s capacity is dedicated to visual perception.
2. The most active muscles in your body are the muscles that move your eyes.
3. The surface tissue of your cornea (the epithelium) is one of the quickest-healing tissues in your body. The entire corneal surface can turn over every 7 days.
4. Your eyes can get sunburned. It is called photokeratitis and it can make the corneal epithelium slough off just like your skin peels after a sunburn.
5. Ommatophobia is the fear of eyes.
6. You blink on average about 15 to 20 times per minute. That blink rate may decrease by 50% when you are doing a visually demanding task like reading or working on a computer – and that’s one reason those tasks can lead to more dry-eye symptoms.
7. Your retinas see the world upside down, but your brain flips the image around for you.
8. If you are farsighted (hyperopia) your eye is short, and if you are shortsighted (myopia) your eye is long.
9. An eyelash has a lifespan of about 5 months. If an eyelash falls out it takes about 6 weeks to fully grow back.
10. One in every 12 males has some degree of “color blindness.”
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided on this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
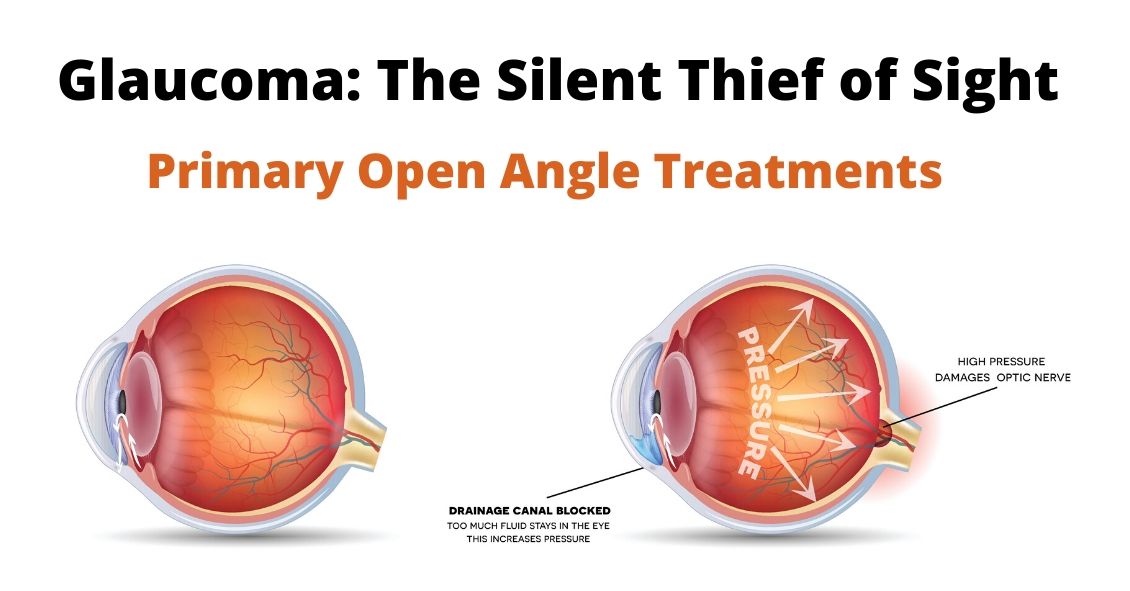
There are several different variations of Glaucoma, but in this article we will mainly focus on Primary Open Angle Glaucoma. This means that there is no specific underlying cause for the Glaucoma like inflammation, trauma, or a severe cataract. It also means that the drainage angle where fluid is drained from the inside of the eye into the bloodstream is not narrow or closed.
Closed or Narrow Angle Glaucoma, which will be discussed in another article, is treated differently from Open Angle Glaucoma
In the U.S., Primary Open Angle Glaucoma (POAG) is by far the most common type of Glaucoma we treat.
Glaucoma is a disease where the Optic Nerve in the back of the eye deteriorates over time, and that deterioration has a relationship to the Intraocular Pressure (IOP). Most - but not all - people diagnosed with Glaucoma have an elevated IOP. Some people have fairly normal IOP’s but show the characteristic deterioration in the Optic Nerve. Regardless of whether or not the pressure was high initially, our primary treatment is to lower the IOP. We usually are looking to try to get the IOP down by about 25% from the pre-treatment levels.
The two mainstays of initial treatment for POAG in the U.S. are medications or laser treatments. There are other places in the world where Glaucoma is initially treated with surgery. However, while surgery can often lower the pressure to a greater degree than either medications or laser treatments, it comes with a higher rate of complications. Most U.S. eye doctors elect to go with the more conservative approach and utilize either medications - most often in the form of eye drops - or a laser treatment.
Drops
There are several different classes of medications used to treat Glaucoma.
The most common class used are the Prostaglandin Analogues or PGA’s. The PGA’s available in the U.S. are Xalatan (latanaprost), Travatan (travapost), Lumigan (bimatoprost) and Zioptan (tafluprost).
PGA’s are most doctors’ first line of treatment because they generally lower the IOP better than the other classes; they are reasonably well tolerated by most people; and they are dosed just once a day, while most of the other drugs available have to be used multiple times a day.
The other classes of drugs include beta-blockers that are used once or twice a day; carbonic anhydrase inhibitors (CAI’s ), which come in either a drop or pill form and are used either twice or three times a day; alpha agonists that are used either twice or three times a day; and miotics, which are used three or four times a day. All of these other medications are typically used as either second-line or adjunctive treatment when the PGA’s are not successful in keeping the pressure down as single agents.
There are also several combination drops available in the U.S. that combine two of the second-line agents (Cosopt, Combigan, and Symbrinza).
Laser
The second option as initial treatment is a laser procedure.
The two most common laser treatments for Open Angle Glaucoma are Argon Laser Trabeculoplasty (ALT) or Selective Laser Trabeculoplasty (SLT). These treatments try and get an area inside the eye called the Trabecular Meshwork - where fluid is drained from the inside of the eye into the venous system - to drain more efficiently.
These treatments tend to lower the pressure to about the same degree as the PGA’s do with over 80% of patients achieving a significant decrease in their eye pressure that lasts at least a year. Both laser treatments can be repeated if the pressure begins to rise again in the future but the SLT works slightly better as a repeat procedure compared to the ALT.
Article contributed by Dr. Brian Wnorowski, M.D.
Yay--It’s 2020!
Maybe it’s not official, but we declare this to be the year of vision care.
Yes, all of us in the eye care community have been hyperventilating, waiting for this year forever! We even heard of at least one optometrist who was putting off retirement because he wanted to be able to practice in 2020. That’s commitment to a pun!
We’re sure you’ll hear a lot of 2020 jokes this year—but at least you’ll see them coming.
Here are a couple more.
Question: Who do we think will win the next Presidential election?
Answer: We don’t know. We don’t have 2020 vision.
Question: What will be the biggest news story of this year?
Answer: Ask us next year. Hindsight is always 2020.
All joking aside though, what better time than the year 2020 to make sure that your vision is where it should be? Get an eye exam, talk with your eye care professional about issues that are troubling you, stop putting off getting your eyes dilated, see if your child’s problems in school could be resolved with a little vision therapy, quit MacGyvering your old glasses with duct tape and a bendy straw. Your vision is one of your greatest treasures—we want to help you treat it that way!
Welcome to 2020—the year of 20/20 vision!
In light of the holiday season, here are our top 10 eye care jokes.
1) What do you call a blind deer? No Eye Deer!
2) What do you call a blind deer with no legs? Still No Eye Deer!
3) Why do eye doctors live long lives? Because they dilate!
4) Why did the blind man fall into the well? He couldn’t see that well.
5) Why shouldn’t you put avocados on your eyes? Because you might get guac-coma!
6) What did the right eye say to the left eye? "Between you and me, something smells."
7) A man goes to his eye doctor and tells the receptionist he’s seeing spots. The receptionist asks if he’s ever seen a doctor. The man replies, “No, just spots.”
8) How many eye doctors does it take to screw in a light bulb? One … or two
9) Unbeknownst to her, a woman was kicked out of peripheral vision club. She didn’t see that one coming!
10) What do you call a blind dinosaur? A do-you-think-he-saurus
Bonus: What do you call a blind dinosaur’s dog? A do-you-think-he-saurus rex!
Article contributed by Dr. Jonathan Gerard

Christmas is one of the most joyful times of the year... thoughts of cookies, decorations, family gatherings, and toys abound. Birthday parties for kids add to the list of wonderful memories as well. But there are a few toys that may not make memories so fun because of their potential for ocular harm. The American Optometric Association lists dangerous toys each year to warn buyers of the potential harm to children’s eyes that could occur because of the particular design of that toy.
Here is a sample of that toy list:
- Laser toys and laser pointers, or laser sights on toy guns pose serious threat to the retina, which may result in thermal burns or holes in the retina that can leave permanent injury or blindness. The FDA’s Center for Devices and Radiological Health issues warnings on these devices at Christmas peak buying times.
- Any type of toy or teenage gun that shoots a projectile object. Even if the ammo is soft pellets, or soft tipped it can still pose a threat. Even soft tipped darts are included in this harmful toy list. A direct hit to the eye can be debilitating.
- Any toy that shoots a stream of water at high velocity can cause damage to the front and or back of the eye. The pressure itself, even though its just water, can damage small cells on the front and back of the eye.
- Any toy that shoots string out of an aerosol can can cause a chemical abrasion to the front of the eye, just as bad as getting a chemical sprayed into the eye.
- Toy fishing poles or toys with pointed edges or ends like swords, sabers or toy wands. Most injuries occur in children under 5 without adult supervision and horseplay can end up in a devastating eye injury from puncture.
The point is, that there are so many great toys to buy for children that can sidestep potential visual harm, that it behooves one to be aware of pitfalls of certain dangerous toy designs.
A great resource of information comes from World Against Toys Causing Harm.
For more information and for this year's list of hazardous toys, visit the W.A.T.C.H. website.
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Your Eyes Are A Precious Gift--Protect Them During The Holidays
“I want an official Red Ryder, carbine action, two-hundred shot range model air rifle!”
“No, you'll shoot your eye out.”
This line from “A Christmas Story” is one of the most memorable Christmas movie quotes ever. Funny in the movie, but the holiday season does present a real eye injury threat.
For those who celebrate Christmas, that risk begins even before the actual day.
Some of the most frequent holiday-related eye injuries come from the Christmas tree itself.
Holiday eye safety begins with the acquisition of the tree. If you are cutting down your own tree, please wear eye protection when doing the cutting--especially if you are going to be using a mechanical saw such as a chain saw or sawzall. You need to also be careful of your eyes when loading a tree on top of the car. It is easy to get poked in the eye when heaving the tree up over your head.
Once back at home, take care to make sure no one else is standing close to the tree if you had it wrapped and now need to cut the netting off. The tree branches often spring out suddenly once the netting is released.
Other injuries occur in the mounting and decorating phase. Sharp needles, pointy lights, and glass ornaments all pose significant eye injury risk. If you are spraying anything like artificial tree snow on the branches be sure to keep those chemicals out of your eyes.
Having now successfully trimmed the tree without injury, let’s move our holiday eye safety talk to the toys.
We want to spend the holiday happily exchanging gifts in front of a warm fire, drinking some eggnog, and snacking on cookies--not going to the emergency room with an injury.
The Consumer Product Safety Commission reported there were 254,200 toy-related emergency room visits in 2015, with 45% of those being injuries to the head and face--including the eyes.
In general, here are the recommendations from the American Academy of Ophthalmology in choosing eye-safe toys for gifts:
- “Avoid purchasing toys with sharp, protruding or projectile parts."
- “Make sure children have appropriate supervision when playing with potentially hazardous toys or games that could cause an eye injury."
- “Ensure that laser product labels include a statement that the device complies with 21 CFR (the Code of Federal Regulations) Subchapter J."
- “Along with sports equipment, give children the appropriate protective eyewear with polycarbonate lenses. Check with your eye doctor to learn about protective gear recommended for your child's sport."
- “Check labels for age recommendations and be sure to select gifts that are appropriate for a child's age and maturity."
- “Keep toys that are made for older children away from younger children."
- “If your child experiences an eye injury from a toy, seek immediate medical attention.”
More specifically, there is a yearly list of the most dangerous toys of the season put out by the people at W.A.T.C.H. (world against toys causing harm).
Here are their 10 worst toy nominees for 2018, with four on the list that are specifically there for potential eye injury risk.
Here are other toys to avoid:
- Guns that shoot ANY type of projectile. This includes toy guns that shoot lightweight, cushy darts.
- Water balloon launchers and water guns. Water balloons fired from a launcher can easily hit the eye with enough force to cause a serious eye injury. Water guns that generate a forceful stream of water can also cause significant injury, especially when shot from close range.
- Aerosol string. If it hits the eye it can cause chemical conjunctivitis, a painful irritation of the eye.
- Toy fishing poles. It is easy to poke the eyes of nearby children.
- Laser pointers and bright flashlights. The laser or other bright lights, if shined in the eyes for a long enough time, can cause permanent retinal damage.
There are plenty of great toys and games out there that pose much lower risk of injury so choose wisely, practice good Christmas eye safety, and have a great holiday season!
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

Many people prefer shopping online to shopping in stores for many of their needs.
With technology constantly improving and evolving, people tend to take advantage of the convenience of shopping online. Whether it’s clothing, electronics, or even food, you can easily find almost everything you need on the Internet.
Eyeglasses, unfortunately, are no different. Many online shops have been popping up in recent years, offering people that same convenience. But what they don’t tell you is that it comes at a price, and this article’s purpose is to shine a light on the negatives of shopping online for eyeglasses.
Here are some important reasons to avoid the temptation of ordering glasses online.
- Accuracy--Instead of saving the most important point for last, we will start with the main reason that ordering eyeglasses online is a bad idea. Product accuracy is a huge reason that the online market has not completely taken off. Every person who needs eyeglasses needs to understand the process for how their prescription is obtained in order to truly understand why shopping online is a bad idea. It is called an eyeglass prescription for a reason. Your eye doctor is prescribing your lenses as if they were prescribing any form of medication. To take that prescription and hand it over to a website that does not require licensed workers to interpret the prescription is not the wisest choice. Equally as important as the prescription itself are the pupillary distance (PD) measurement, and the optical centers. These measurements are often not given at the time of the examination, but instead are administered by the optician at the point of sale. Not having these measurements done accurately will negatively affect the quality of vision as much as an error in the prescription.
- Quality--Similar to the accuracy of the lens, the quality of the product you are purchasing is affected when making the decision to purchase online. The saying “too good to be true” is the case more times than not, and this purchase is no exception. When you see enticing advertisements for pricing that seems to be too good, there is a reason. This product is often not inspected or handled by a state-licensed optician. These websites rely on mass production in order to operate. Factory workers operating machines pale in comparison to the experience you will receive in a professional office. Skilled opticians licensed to interpret and manufacture your eyeglass prescriptions are held to a much higher standard than factory workers.
- Warranty--Due to their low prices, many of these websites do not include any form of product warranty or guarantee. Opticians, however, stand behind your purchase. If there are issues with adjustment or a patient not being comfortable in a specific lens or product, professional opticians are willing to work with you. This personal experience is not attainable on the web.
- Coordination with your doctor--With the complexity of eyeglass lenses, the ease of working in-house or with a nearby lab is always a benefit worth keeping in mind. Eyeglass lenses can be very complex products. Having the benefit of being able to work directly with the doctor gives the optician the best chance to put you in the exact lenses you need. There is a substantial difference in the percentage of error between shopping online and buying from a local private practice.
- Personal Experience--Probably the most important factor for many people, the personal experience you get when shopping in person is something you cannot obtain by using the Internet. Dealing with the same opticians year in and out is something patients emphasize and appreciate. Just like people tend to keep the same doctors over the years, patients like knowing that the same people will be in charge of making their glasses. Shopping online does not offer that experience.
All of these factors should be carefully considered when making the decision where to buy glasses. While the initial price difference could entice you online at first, know that it does come at a price. Warrantied product, quality, and convenience are very important factors when buying glasses. People sometimes tend to discount just how intricate eyeglasses prescriptions and fit really are.
Article contributed by Richard Striffolino Jr.
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ

No this is not a late-night personal injury lawyer infomercial.
This is a recommendation that you have your LASIK records available, for your own good, later in life.
There are 2 million cataract surgeries done yearly in the U.S. and the odds are, if you live long enough, you will eventually need cataract surgery, too.
What does this have to do with LASIK surgery?
When doctors perform cataract surgery we remove the cataract, which is the lens of your eye that has become cloudy. And we replace that lens with an artificial lens called an Intraocular Lens implant (IOL).
The IOL needs to have a strength to it to match your eye so that things are in focus without the need for strong prescription eyeglasses.
Currently, we determine what the strength the IOL needs to be by using formulas that mostly depend on the measurements of the curvature of the cornea and the length of the eye.
Those formulas work best when the cornea is its natural shape - i.e., not previously altered in shape after LASIK.
If you plug the “new” post-LASIK corneal shape into the formulas, the IOL strength that comes out is often significantly off the strength you really need to see well.
This is where having your records becomes important.
Knowing what your eyeglass prescription and corneal shape was BEFORE you had LASIK greatly improves our formula’s ability to predict the correct implant strength.
In most states there is a limit to how long a doctor needs to keep your records after your last visit, so everyone who has had LASIK surgery should get a copy of your pre- and post-LASIK records NOW before they no longer exist.
Article contributed by Dr. Brian Wnorowski, M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.
Read more: Why everyone who has had LASIK surgery should get their records NOW

Diabetic retinopathy, which is a complication of diabetes that affects the eyes, is detected during a comprehensive eye exam that includes:
- Visual acuity testing.
- Dilated exam in which drops are placed to widen the pupil to allow examination of the retina.
- Tonometry. Measurement of the eye pressure inside the eye.
Supplemental testing may include:
- Optical coherence tomography (OCT). This is a non-invasive test that images the retina to detect any fluid or diabetic macular edema.
- Fluorescein Angiography. This test involves an injection of a dye into your arm and a series of pictures that are taken as the dye flows through the retinal vessels. This may show leakage of fluid or the growth of new blood vessels in the retina.
Treatment for Diabetic Retinopathy
The best treatment is prevention of diabetic retinopathy by strict control of blood sugars. Once diabetic retinopathy is present, treatment of diabetic retinopathy will slow progression but won’t cure it.
Diabetic macular edema can be treated with several different therapies that may be used alone or in combination.
These include:
- Injection therapy. Anti-VEGF drugs are injected into the eye to block a substance called vascular endothelial growth factor (VEGF). This medication will block abnormal blood vessel growth and decrease the leakage of fluid into the retina. The three most commonly used drugs include Avastin, Lucentis and Eylea. Steroids are another option for treatment of diabetic macular edema but are used less often due to side effects of possible cataracts and increased eye pressure.
- Laser therapy. Small laser burns are applied in the area of the retinal swelling to slow the leakage of fluid. Laser treatment can be combined with anti-VEGF injections.
Proliferative diabetic retinopathy can be treated with:
- Laser therapy. Laser is applied on the retina to shrink the new blood vessels and to prevent bleeding inside the eye. Bleeding inside the eye will cloud the vision and cause floaters, which are small moving spots that appear in your field of vision.
- Surgery. When there is significant amount of blood or scar tissue inside the eye, then a vitrectomy surgery is performed to remove the blood and scar tissue. Laser and anti-VEGF therapy may also be applied during the surgery.
In the end, the best treatment is prevention of diabetic retinopathy. An annual comprehensive dilated eye exam is recommended for anyone who has been diagnosed with diabetes, since early mild non-proliferative diabetic retinopathy can show no symptoms.
Article contributed by Jane Pan M.D.
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ

Transition lenses in eyeglasses have been around for many years now. The mechanics behind transition lenses is that certain chemicals in the lens interact with UV light from the sun and turn the lenses dark when you go outside and back to clear when you go inside.
This is a great accompaniment to sunglasses, as it is not always convenient to be carrying around multiple pairs of glasses with you, especially when going from inside to outside frequently. However, there are some drawbacks to transitions, including the fact that they don’t get as dark as sunglasses, have some difficulty turning dark in the car, and have a tendency to keep a slight constant tint even in dark conditions.
Vistakon, the optical wing of Johnson & Johnson, has come out with the first transition contact lens. Acuvue Oasys Transitions hit the market recently and while it is still brand-new technology, preliminary results have been generally positive.
Just a couple personal thoughts: It looks a little strange. The material itself turns a dark shade of grey and therefore the person is walking around with eyes that look black. On the plus side, though, this would be good for people limited by high prescriptions and who have difficulty with peripheral vision and glasses, yet still want the transition technology. On the other hand, wearing clear contact lenses with sunglasses would provide better sun coverage with the ability to remove the sunglasses when desired.
There is one other area where transition contacts might become very useful and that is in outdoor sports. For any athlete who is playing an outdoor sport where the lighting conditions may change from day to day or even within a single game or event, these contacts may significantly improve the ability to perform. This is especially true in any sport where there may be significant contact or rapid head movement that can make it difficult to compete in sunglasses.
While in its infancy, transition contact lenses look to be a promising technology.
Article contributed by Dr. Jonathan Gerard
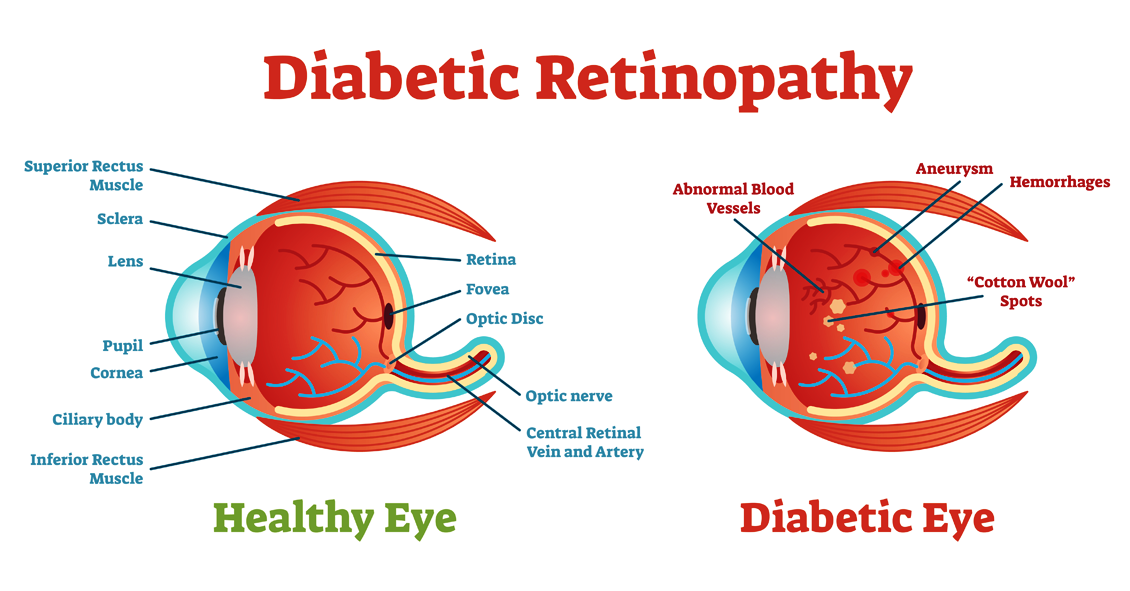
Diabetic retinopathy is an eye condition that affects the retina in people who have diabetes.
The retina is the light-sensitive tissue that lines the back of the eye, and detects light that is then processed as an image by the brain. Chronically high blood sugar or large fluctuations in blood sugar can damage the blood vessels in the retina. This can result in bleeding in the retina or leakage of fluid.
Diabetic retinopathy can be divided into non-proliferative or proliferative diabetic retinopathy.
Non-proliferative diabetic retinopathy: In the early stage of the disease, there is weakening of the blood vessels in the retina that causes out-pouching called microaneurysms. These microaneurysms can leak fluid into the retina. There can also be yellow deposits called hard exudates present in the retina from leaky vessels.
Diabetic macula edema is when the fluid leaks into the region of the retina called the macula. The macula is important for sharp, central vision needed for reading and driving. The accumulation of fluid in the macula causes blurry vision.
Proliferative diabetic retinopathy: As diabetic retinopathy progresses, new blood vessels grow on the surface of the retina. These blood vessels are fragile, which makes them likely to bleed into the vitreous, which is the clear gel that fills the middle of the eye. Bleeding inside the eye is seen as floaters or spots. Over time, scar tissue can then form on the surface of the retina and contract, leading to a retinal detachment. This is similar to wallpaper contracting and peeling away from the wall. If left untreated, retinal detachment can lead to loss of vision.
Symptoms of diabetic retinopathy:
- Asymptomatic: In the early stages of mild non-proliferative diabetic retinopathy, the person will usually have no visual complaints. Therefore, it is important for people with diabetes to have a comprehensive dilated exam by their eye doctor once a year.
- Floaters: This is usually from bleeding into the vitreous cavity from proliferative diabetic retinopathy.
- Blurred vision: This can be the result of fluid leaking into the retina, causing diabetic macular edema.
Risk factors for diabetic retinopathy:
- Blood sugar. Lower blood sugar will delay the onset and slow the progression of diabetic retinopathy. Chronically high blood sugar and the longer the duration of diabetes, the more likely chance of that person having diabetic retinopathy.
- Medical conditions. People with high blood pressure and high cholesterol are at greater risk for developing diabetic retinopathy.
- Ethnicity. Hispanics, African Americans and Native Americans are at greater risk for developing diabetic retinopathy.
- Pregnancy. Women with diabetes could have an increased risk of developing diabetic retinopathy during pregnancy. If they already have diabetic retinopathy, it might worsen during pregnancy.
Article contributed by Jane Pan M.D.
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ
In our modern world, people spend hours on end staring at computer screens, smartphones, tablets, e-readers, and books that require their eyes to maintain close focus.
For most people (all except those who are nearsighted and aren’t wearing their glasses), their eyes’ natural focus point is far in the distance. In order to move that focus point from far to near there is an eye muscle that needs to contract to allow the lens of the eye to change its shape and bring up-close objects into focus. This process is called accommodation.
When we accommodate to view close objects, that eye muscle has to maintain a level of contraction to keep focused on the near object. And that muscle eventually gets tired if we continuously stare at the near object. When it does, it may start to relax a bit and that can cause vision to intermittently blur because the lens shape changes back to its distance focal point and the near object becomes less clear.
Continuing to push the eyes to focus on near objects once the focus starts to blur will began to produce a tired or strained feeling in addition to the blur. This happens very frequently to people who spend long hours reading or looking at their device screens.
An additional problem that occurs when we stare at objects is that our eyes’ natural blink rate declines. The average person blinks about 10 times per minute (it varies significantly by individual) but when we are staring at something our blink rate drops by about 60% (4 times per minute on average). This causes the cornea (the front surface of the eye) to dry out faster. The cornea needs to stay moist in order to see clearly, otherwise little dry spots start appearing in the tear film and the view gets foggy. Think about your view through a dirty car windshield and how much that view improves when you turn the washers on.
So what should you do if your job, hobby or passion requires you to stare at a close object all day?
Follow the 20-20-20 rule. Every 20 minutes, take 20 seconds and look 20 feet into the distance. This lets the eye muscle relax for 20 seconds, and that is generally enough for it to have enough energy to go back to staring up close for another 20 minutes with much less blurring and fatigue. It also will help if you blink slowly several times while you are doing this to help re-moisten the eye surface.
Don’t feel like you can give up those 20 seconds every 20 minutes? Well if you don’t, there is evidence that your overall productivity will decline as you start suffering from fatigue and blurring. So take the short break and the rest of your day will go much smoother.
Article contributed by Dr. Brian Wnorowski, M.D.
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ

Fall brings a lot of fun, with Halloween bringing loads of it.
But did you know that some Halloween practices could harm your vision? Take Halloween contacts, for instance. They vary widely, with everything from monster eyes to goblin eyes to cat eyes to sci-fi or a glamour look. They can be just the added touch you need for that perfect costume. However, some people do not realize that the FDA classifies contact lenses as a medical device that can alter cells of the eye and that damage can occur if they are not fit properly.
Infection, redness, corneal ulcers, hypoxia (lack of oxygen to the eye) and permanent blindness can occur if the proper fit is not ensured. The ICE, FTC, and FDA are concerned about costume contacts from the illegal black market because they are often unsafe and unsanitary. Proper safety regulations are strictly adhered to by conventional contact lens companies to ensure that the contact lenses are sterile and packaged properly and accurately.
Health concerns arise whenever unregulated black-market contacts come into the US market and are sold at flea markets, thrift shops, beauty shops, malls, and convenience stores. These contacts are sold without a prescriber's prescription, and are illegal in the US. There have also been reports of damage to eyes because Halloween spook houses ask employees to share the same pair of Halloween contact lenses as they dress up for their roles.
So the take home message is, have a great time at Halloween, and enjoy the flare that decorative contacts can bring to your costume, but get them from a reputable venue and be fit by an eye care professional with a proper legal prescription. Don't gamble with your eyes for a night of Halloween fun!
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ

The tears that coat the surface of your eyes have both a liquid and a mucous layer to them. It is normal to have a very thin amount of mucus in your tear film. But that mucus can significantly increase when the eye gets irritated.
Some of the most common causes of irritation that can make the eye overproduce mucus are:
- Conjunctivitis, which could be caused by an allergy, bacteria or virus
- Blepharitis, which is an inflammation of the eyelids
- Dry Eye
When any of these conditions occur, the eye will begin to make more mucus.
Sometimes the mucous production really is excessive and there is a temptation to keep pulling it out with either your fingers or a cotton swab. Don’t do it; it just leads to recurring irritation and problems.
Any mucus that gets deposited OUTSIDE the eye on the outer eyelid or on the lashes is fair game for removal. In fact, anything on the exterior of the eyelid or stuck to the eyelashes should be cleaned off. Just don’t reach INSIDE the eyelids.
Every time you go in there to pull out mucus, your finger or a cotton swab further irritates the eye and causes it to make more mucus and you end up with the viscious cycle that we call mucus fishing syndrome.
If you have an acute problem that is causing excessive mucus, you need to try and get the underlying problems treated and under control. That means treating the allergy, blepharitis, infectious conjunctivitis, or Dry Eye.
In addition, you need to STOP putting your fingers in your eye and pulling the mucus out. Sit on your hands if you have to but you have to stop or it is never going to get better.
If you are through treatment for the original problem but still find yourself pulling mucus out of your eye you may need your doctor to try a steroid drop in order to decrease the production and try to help you get out of the habit of putting your fingers in your eyes.
Article contributed by Dr. Brian Wnorowski, M.D.
Shingles is the term we use to describe a condition that is caused by a re-activation of the Herpes Varicella-Zoster virus. The origin of this infection usually goes way back to childhood with a disease we know as “chickenpox.”
When you have a chickenpox infection your immune system manages to eventually suppress that virus from causing an active infection, but the virus does not get completely eliminated from your body--it is able to go and hide in your nerve roots.
Your immune system manages to keep the virus in check for most of your life but there may come a time in adulthood when your immune system is not working as well as it used to, and the virus can reappear. It usually does this along the distribution of a single sensory nerve called a dermatome.
The most common area for this to occur is along your trunk (chest or abdomen) but it is also commonly found on the face.
There are three branches of nerves that supply sensation to your face. They are all branches of the fifth cranial nerve. Those three branches supply the upper face (V1), the mid face (V2), and the lower face (V3). Most of the time, shingles breaks out along only one of the branches at a time. The one that most frequently involves the eye is a rash breakout in the V1 distribution. This can involve the forehead and both the upper and lower eyelid. It is also much more likely that the inside of the eye will be involved if the tip of the nose has a lesion on it. The reason for that is that there is a specific subbranch of the V1 nerve called the nasocilliary nerve. This nerve is responsible for sensation on the tip of the nose and the inside of the eye.
The hallmark of shingles is that once the rash erupts it stays on one side of the body, including when it happens on the face. The rash will go up to the centerline of your face but will not go to the other side. You may get lesions on your scalp, but they will not show up on the back of your head. That is because the V1 does not go past half way back on your scalp. The back of your head has its sensation handled by nerves that come out of your spinal cord not cranial nerves that come out of the front of your skull.
Many people have a hard-to-describe sensation of pain, irritation, or itching along the distribution of the nerve for a day or two before the rash shows up. It is important to recognize the rash as quickly as possible because the drugs that treat shingles--usually Acyclovir, Famvir (famciclovir), or Valtrex (valacyclovir)--are much more effective if they are started within three days of the beginning of the rash.
Eye problems may occur along with the rash, especially if there is a lesion on the tip of the nose.
The two biggest problems are swelling or inflammation of the cornea and inflammation inside the eye, which we call iritis or uveitis.
The inflammation in the eye can cause pain and it can also increase the eye pressure and cause glaucoma. Most often the treatment for the eye problem is to use the same oral medication mentioned above and sometimes it also can require eye drops to decrease the inflammation the virus is causing (steroid drops) or drops to try and lower the elevated pressure (glaucoma drops).
The eye inflammation can cause blurred vision, pain, and significant light sensitivity. It can be hard to treat and control and can continue to be a problem long after the skin lesions are gone. In fact, many times problems don’t even start until the skin lesions are starting to go away.
It is recommended that if you have shingles effecting the distribution of V1 that you have an eye exam within a few days of the diagnosis being made and then again a week later because, as mentioned above, the eye problems can present a week later than the skin eruptions.
There can be some serious long-term effects of shingles on your eye including glaucoma and corneal scarring that can be bad enough to require a corneal transplant. The symptoms are often obvious with the vision being blurry and the eye being very red and painful, but sometimes the symptoms may be much more mild even when significant trouble is brewing inside the eye. So even if you think the eye feels fine, you need an exam to ensure there is not subtle inflammation or significant elevation of the pressure in the eye.
The other long-term problem with shingles around the eye is the possibility of there being ongoing pain in the area that can last for many years. This is called Post Herpetic Neuralgia (PHN). This pain can occur all along the dermatome where shingles had occurred. The eye itself may look perfectly normal but the pain persists. This is often treated with drugs that were originally developed as seizure medication but have since been shown to help alleviate neurological pain. The two most commonly used drugs for this are Neurontin (Gabapentin) and Lyrica (Pregabalin).
The most important thing you can do to try and make sure this doesn’t happen to you is to be vaccinated for shingles. The original vaccination called Zostavax has been available since 2006 in the U.S. It is a single-injection vaccine and was recommend for everyone over 60. The main issue with this vaccine is that it only reduced the risk of getting shingles by 51% and PHN by 67%. In 2017 a new vaccine was approved in the U.S. called Shingrix. This vaccine is a two-injection vaccine with the second shot given 2 to 6 months after the first. This vaccine is recommended for everyone 50 years or older. The big advantage of this vaccine is that is 90% effective in preventing both shingles and PHN. There have been some shortages of this vaccine since its introduction so it may take a while to get it but you should definitely do it when it is available. For more information about this vaccine you can go to the CDC website by clicking here.
Article contributed by Dr. Brian Wnorowski, M.D.

Lyme disease is an infection that is caused by a spirochete (a type of microorganism) called Borrelia burgdorferi. It is transmitted to humans by the bite of a deer tick.
The disease has a strong geographical incidence, being highly concentrated in the Northeast United States and now also has a high incidence in Minnesota and Wisconsin.
Lyme disease was first discovered in Old Lyme, Connecticut in 1975. It can start with a characteristic “bull’s eye” rash, in which there is a central spot that is surrounded by clear skin that is then ringed by an expanding rash. It can also appear just as an expanding rash.
This rash usually starts within days of the tick bite. Eye problems can occur along with this rash in the first phase of the disease. This includes red eyes that can look like full-blown pink eye, along with eyelid swelling. It also can produce iritis or uveitis, which include sensitivity to light and inflammation inside the eye.
The second phase of the disease usually starts within a few weeks of the tick bite and this occurs because the spirochete gets into the blood stream. This stage often has rashes starting away from the original bite site. It can also produce joint pain, weakness, and inflammation in several organs including the heart, spleen, liver and kidneys.
There are also several ways it can affect your eyes. It can cause inflammation in your cornea (keratitis), retina (retinitis), optic nerve (optic neuritis), uveitis, inflammation in the jelly-like substance that fills the back of the eye called vitreous (vitritis) and the muscles that move your eye around (orbital myositis). It can also affect the eye if it causes problems with the nerve that controls your eyelid muscles so that your eye will not close properly (Bell’s palsy).
There is a third phase of the disease that is caused by long-term persistent infection. This phase can create multiple neurologic problems and can appear very similar to the presentation of Multiple Sclerosis (MS). The eyes can show any of the same signs as phase two, but the most common presentation is persistent keratitis.
The diagnosis is made by observing the presenting symptoms, being in an area where there are significant numbers of the disease-carrying ticks, and a blood test that can confirm the diagnosis.
The symptoms and signs of Lyme Disease can mimic many other problems, so it is important to keep Lyme Disease in mind if you are having multiple problems involving different organs and you know or have any suspicion that you may have had a tick bite while you were in areas where the disease is prevalent.
Article contributed by Dr. Brian Wnorowski, M.D.
Did you know that having one's eyes tested can reveal symptoms of ADHD (Attention Deficit Hyperactivity Disorder)? ADHD is a set of symptoms that include trouble with focus, overactivity, and behavioral control. It is estimated that one in five people has some sort of ADHD.
ADHD is a condition that has multiple symptoms and it can affect any age, though commonly it affects children. There is difficulty with visual processing, which includes doubling letters, reversing letters, jumping words and lines of print.
Eye examinations are a crucial part of the diagnosis of ADHD. Proper visual function can be assessed through a thorough eye exam. During the exam, visual complaints, focusing, and processing can be assessed to rule out ADHD.
When glasses are prescribed for an patient with ADHD, prescribing the correct type of lens is vital. Many patients benefit from an anti-glare/anti-reflective or AR treatment on their lenses. This cuts unnecessary light from entering the eye, making visual processing easier.
In some cases, it is discovered that the person has a non-ocular visual processing problem. This simply means that their eyes have little or nothing to do with the symptoms of ADHD. This gives valuable information to the health care provider that is managing the patient and suggests more non-ocular testing for a compete diagnosis.
ADHD is very common, and the great news is there are many treatment options. Many resources for help are available on the Internet and through health care channels.
Having an eye exam should be one of the first items on the checklist if you are suspicious about ADHD because valuable information on visual processing can be gained.
For more resources see these websites:
National Institute of Mental Health, www.nimh.nih.gov/
American Optometric Association, AOA.org
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.

There are many things that can cause your eye to turn red.
The eye looks red when the blood vessels that are in the conjunctiva (the mucous membrane that covers the white of your eye and the backside of your eyelids) becomes dilated.
Those blood vessels often dilate when the eye gets irritated. This irritation can originate from a problem occurring inside the eye or factors from outside the eye.
The most common external factors that can cause the eye to become red are exposure to infectious organisms (mostly viruses and bacteria), environmental irritants (smoke, chemicals, sunlight), or allergens.
Infectious organisms can cause infectious conjunctivitis, or what is more commonly referred to as “pink eye.” This condition often presents with the eye being red and a mucous discharge being produced, often to such a degree that the eyelids are crusted over upon awaking in the morning. Infectious conjunctivitis can be extremely contagious and it is often advised that you severely limit your exposure to others while the problem is active. Infectious conjunctivitis caused by bacteria can be treated with antibiotic eye drops but viral conjunctivitis currently has no treatment and must run its course like the common cold.
Environmental irritants can make the eye look red for a short period of time during and immediately after exposure. The irritation is usually self-limited but may resolve more quickly with the use of over-the-counter lubricating drops or artificial tears. It is very important to understand exactly which irritant you were exposed to because there are some chemicals (acids and bases) that can cause extreme damage to the eye. So if you’re exposed to a caustic chemical you need to immediately rinse your eye out with water and seek emergency medical attention.
Allergens can cause allergic conjunctivitis, which can look very similar to pink eye but usually has significantly less mucous discharge and is usually accompanied by fairly severe itching. Allergic conjunctivitis is not contagious and can usually be treated with anti-allergy eye drops.
Infectious and allergic conjunctivitis can cause mild discomfort and itching but they rarely cause significant pain or loss of vision. A red eye with significant pain, especially when accompanied by severe light sensitivity and vision loss, often indicates more significant problems such as iritis, angle closure glaucoma or a corneal ulcer, all of which require immediate medical attention. If your eye is red and there is significant pain do not assume you have pink eye--see your eye doctor immediately!
Article contributed by Dr. Brian Wnorowski, M.D.
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ

Dry eye is a very common problem that affects women more than men and becomes more prevalent as people get older.
It can present in many ways, with symptoms that can include a foreign body sensation, burning, stinging, redness, blurred vision, and dryness. Tearing is another symptom and occurs because the eye initially becomes irritated from the lack of moisture and then there is a sudden flood of tears in response to the irritation.
Unfortunately, this flood of tears can wash out other important components of the tear film that are necessary for proper eye lubrication. Signs and symptoms can range from mild to severe.
There are medications that have the potential to worsen the symptoms of dry eye. Here are the broad categories and specific medications that have been known to potentially worsen the symptoms:
- Blood Pressure Medications - Beta blockers such as Atenolol (Tenormin), and diuretics such as Hydrochlorothiazide.
- GERD (gastro-esophageal reflux disorder) Medications - There have been reports of an increase in dry eye symptoms by patients on these medications, which include Cimetidine (Tagamet), Rantidine (Zantac), Omerprazole (Prilosec), Lansoprazole (Prevacid), and Esomeprazole (Nexium).
- Antihistamines - More likely to cause dry eye: Diphenhydramine (Benadryl), loratadine (Claritin). Less likely to cause dry eye: Cetirizine (Zyrtec), Desloratadine (Clarinex) and Fexofenadine (Allegra). Many over-the-counter decongestants and cold remedies also contain antihistamines and can cause dry eye.
- Antidepressants - Almost all of the antidepressants, antipsychotic, and anti-anxiety drugs have the propensity to worsen dry eye symptoms.
- Acne medication - Oral Isotretinoin.
- Hormone Replacement Therapy - The estrogen in HRT has been implicated in dry eye.
- Parkinson's Medication - Levodopa/Carbidopa (Synamet), Benztropine (Cogentin), Procyclidine (Kemadrin).
- Eye Drops - In addition to oral medications many eye drops can actually increase the symptoms of dry eye, especially drops with the preservative BAK.
If you are suffering from dry eye and are using any of the medications above you should discuss this with your eye doctor and medical doctor. Don't stop these medications on your own without consulting your doctors.
Article contributed by Dr. Brian Wnorowski, M.D.
The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ
Parkinson’s disease is a progressive degenerative condition of the neurological system. The majority of Parkinson’s effects are on movement, often starting off very slowly and subtly. One of the earliest symptoms is a slight tremor in one or both hands. Other early symptoms include a lack of facial expression and decreased blinking of the eyes, so it looks like the person is always staring.
The next stage usually results in difficulty with initiating movement, especially walking. It frequently looks like it takes a tremendous concentrated effort to initiate walking and the steps often start off very small with a shuffling of the feet. At the same time, the disease stiffens the muscles of the arms so that when the person is walking there is a noticeable decrease in the swinging of the arms. Speech becomes much softer and writing becomes more of an effort, with handwriting getting smaller and smaller as the disease progresses.
Parkinson’s can also affect your visual performance, mainly in two parts of your eyes: the tear film and the ocular muscles.
It affects your tear film because of the decreased rate of blinking. The tear film is an important component of your optical system. It coats the surface of the cornea and if it is not smooth and uniform the result is a blurring of your vision. Blinking helps refresh your tear film and spreads it out uniformly. It is analogous to the washers and wipers on your car. If the windshield (like your cornea) is spotty you have a hard time seeing through that windshield. Turn on the washers and now there is more moisture on the surface but that is also spotty and hard to see through until the wipers go by and spread the moisture out evenly. That is very similar to how your cornea, tear film and your eyelids blinking interact to keep your vision clear.
If you don’t blink enough, the tear film begins to dry out in spots and having dry spots next to moist spots results in an irregular film and therefore blurred vision. That is how the decreased blinking frequency in people with Parkinson’s disease results in a complaint of intermittent blurred vision.
The other way the disease affects your vision is by creating a problem called convergence insufficiency. When you read, your two eyes turn inward toward each other in a process called convergence. Your eye muscles are activated in order to have the two eyes point inward to focus on the near object. By interfering with the interaction between your nerves and muscles, Parkinson’s makes it difficult to both initiate and sustain the convergence you need to keep both eyes focused on a near object.
This sometimes results in a disconnect between what a person is capable of reading on an eye chart for a short period of time and what happens after trying to sustain the effort over a longer period of time. This disconnect can result in some frustration. Often during an exam, a quick look at the distance eye chart allows the patient to see fairly well because the dry eye may not be causing any blurring if the patient just blinked a few times before reading the chart. A patient may also do well on the near chart because they are often being tested one eye at a time. When you read things up close with just one eye there is no need for the eyes to converge so they do well one eye at a time.
There are some other less-frequent eye problems that can occur with Parkinson’s. One is called blepharospasm, where the eyelids on either one side or both forcefully close involuntarily. A person can also end up with a condition called apraxia of eye opening, where they can’t voluntarily open the eyelids. This is different from blepharospasm because in this condition the lids are not being forcefully closed, they just won’t open when you want them to.
The majority of these problems do improve if the Parkinson’s is treated with medication or even brain stimulation.
Article contributed by Dr. Brian Wnorowski, M.D.

